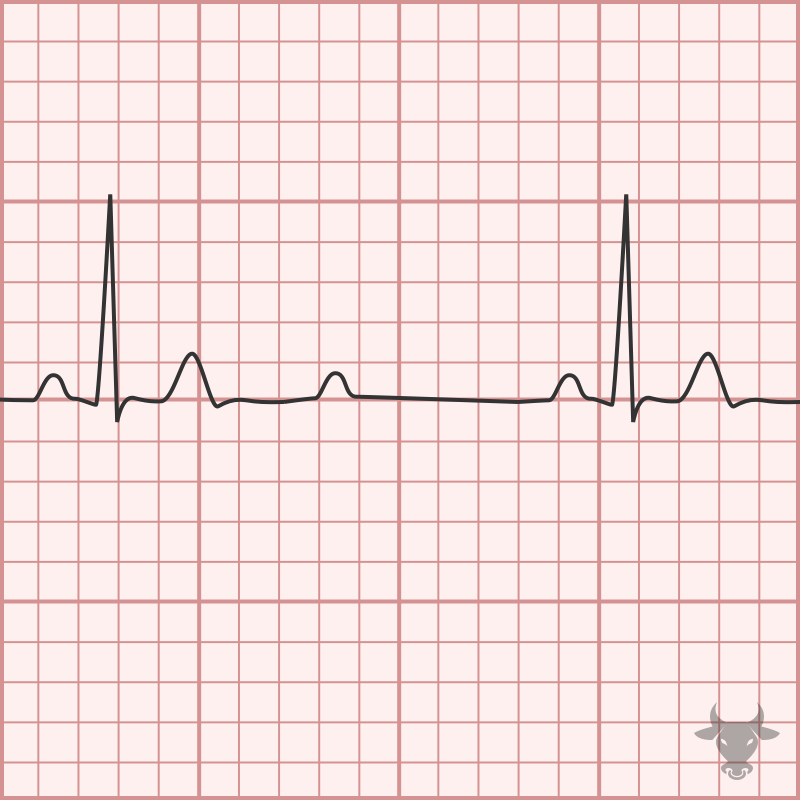
With 2:1 atrioventricular block, it is impossible to know whether it is Mobitz I (nodal) or Mobitz II (infranodal) based on the surface ECG; therefore, 2:1 AV block is simply referred to as “2:1 AV block.” When the QRS is narrow, as in this case, Mobitz I is more likely; however, it is prudent to assume the worst scenario (i.e., Mobitz II).
Second Degree Atrioventricular Block 2:1
Examples
Second Degree Atrioventricular Block 2:1
P waves are conducted in a 2:1 ratio, with every other P wave “dropped”, or failing to conduct through the atrioventricular (AV) node. When P waves are conducted but intermittently “dropped,” it is referred to as second degree AV block, which comes in two varieties - Mobitz I (or Wenckebach) and Mobitz II. Mobitz I occurs when conduction is progressively delayed through the AV node and eventually fails. It is represented by progressively prolonging PR intervals followed by a “dropped” P wave. It does not always represent pathology, particularly when seen in younger or physically fit individuals with high vagal tone. Mobitz II occurs when the infranodal conduction system intermittently fails, resulting in intermittently “dropped” P waves but consistent PR intervals when conducted. Mobitz II usually occurs with preexisting conduction disease (e.g., combination of bundle branch and fascicular blocks), is always pathologic, and more likely to progress to complete heart block. When AV block occurs in a 2:1 ratio, it is impossible to distinguish between Mobitz I and Mobitz II; therefore, 2:1 AV block is simply referred to as “2:1 AV block.” When the QRS is narrow, Mobitz I is more likely; however, it is prudent to assume the worst scenario (i.e., Mobitz II).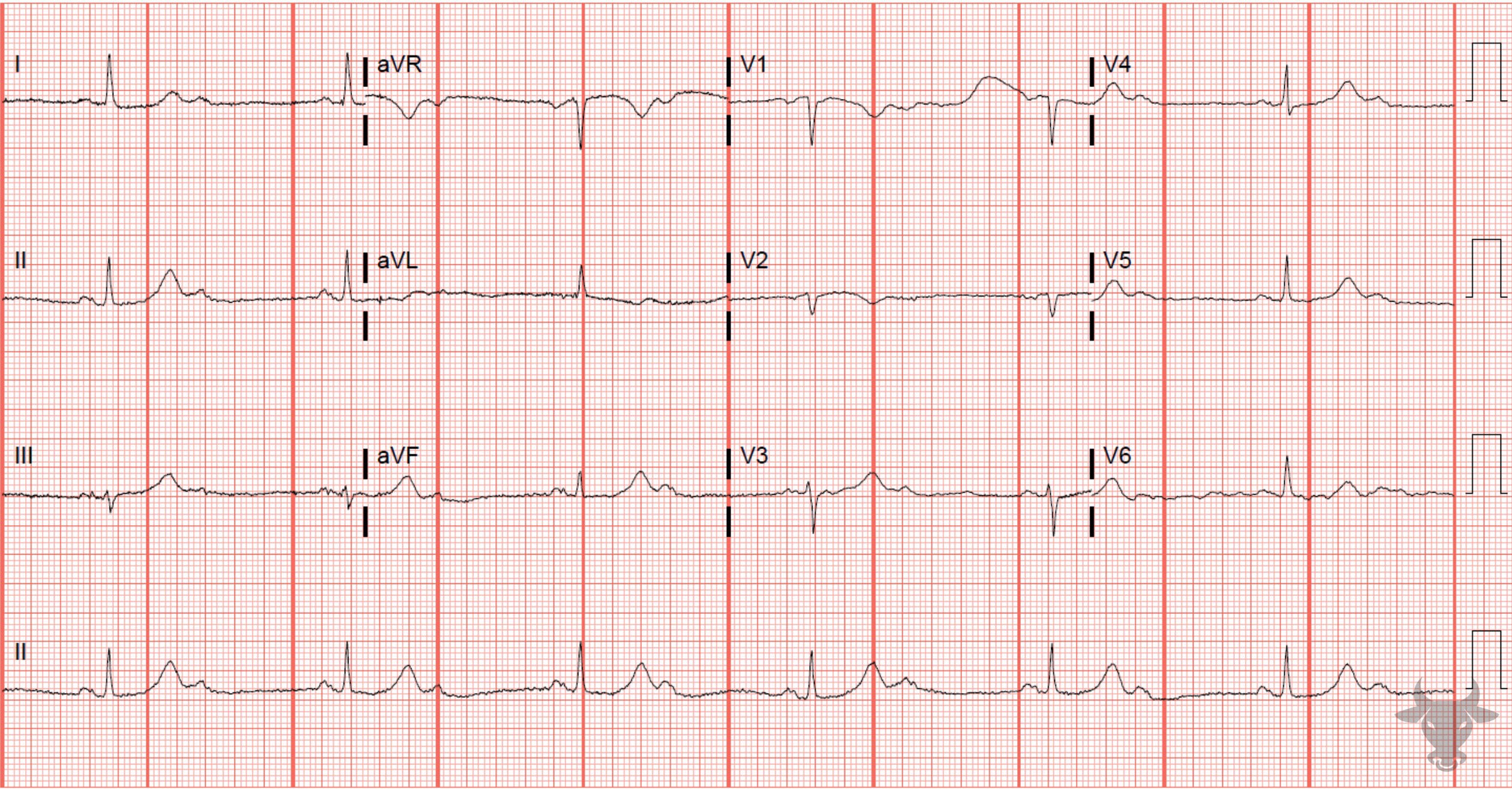
Second Degree Atrioventricular Block 2:1
P waves are conducted in a 2:1 ratio, with every other P wave “dropped”, or failing to conduct through the atrioventricular (AV) node. When P waves are conducted but intermittently “dropped,” it is referred to as second degree AV block, which comes in two varieties - Mobitz I (or Wenckebach) and Mobitz II. Mobitz I occurs when conduction is progressively delayed through the AV node and eventually fails. It is represented by progressively prolonging PR intervals followed by a “dropped” P wave. It does not always represent pathology, particularly when seen in younger or physically fit individuals with high vagal tone. Mobitz II occurs when the infranodal conduction system intermittently fails, resulting in intermittently “dropped” P waves but consistent PR intervals when conducted. Mobitz II usually occurs with preexisting conduction disease (e.g., combination of bundle branch and fascicular blocks), is always pathologic, and more likely to progress to complete heart block. When AV block occurs in a 2:1 ratio (Figure 2), it is impossible to distinguish between Mobitz I and Mobitz II; therefore, 2:1 AV block is simply referred to as “2:1 AV block.” When the QRS is narrow, as in this case, Mobitz I is more likely; however, it is prudent to assume the worst scenario (i.e., Mobitz II).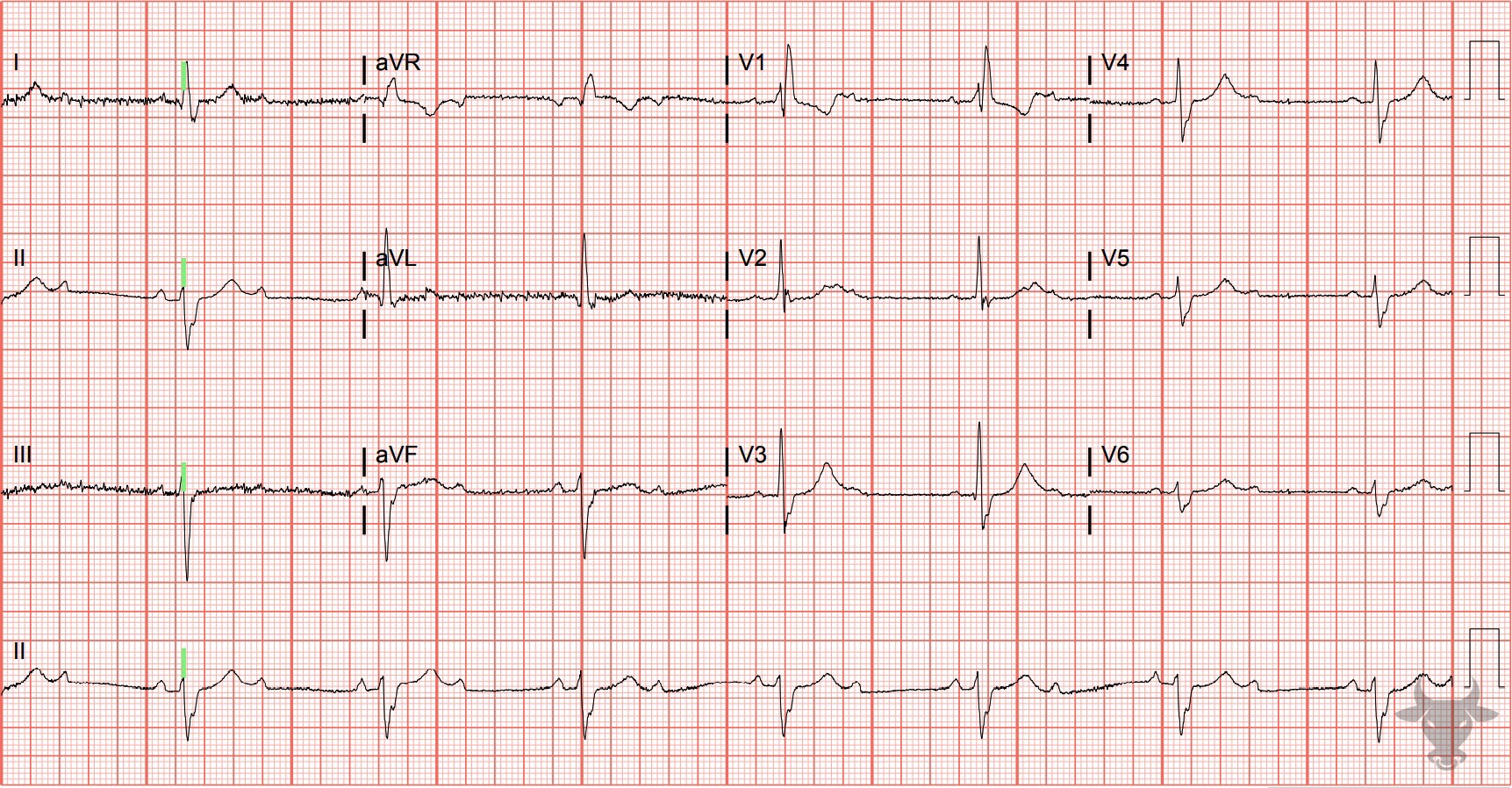
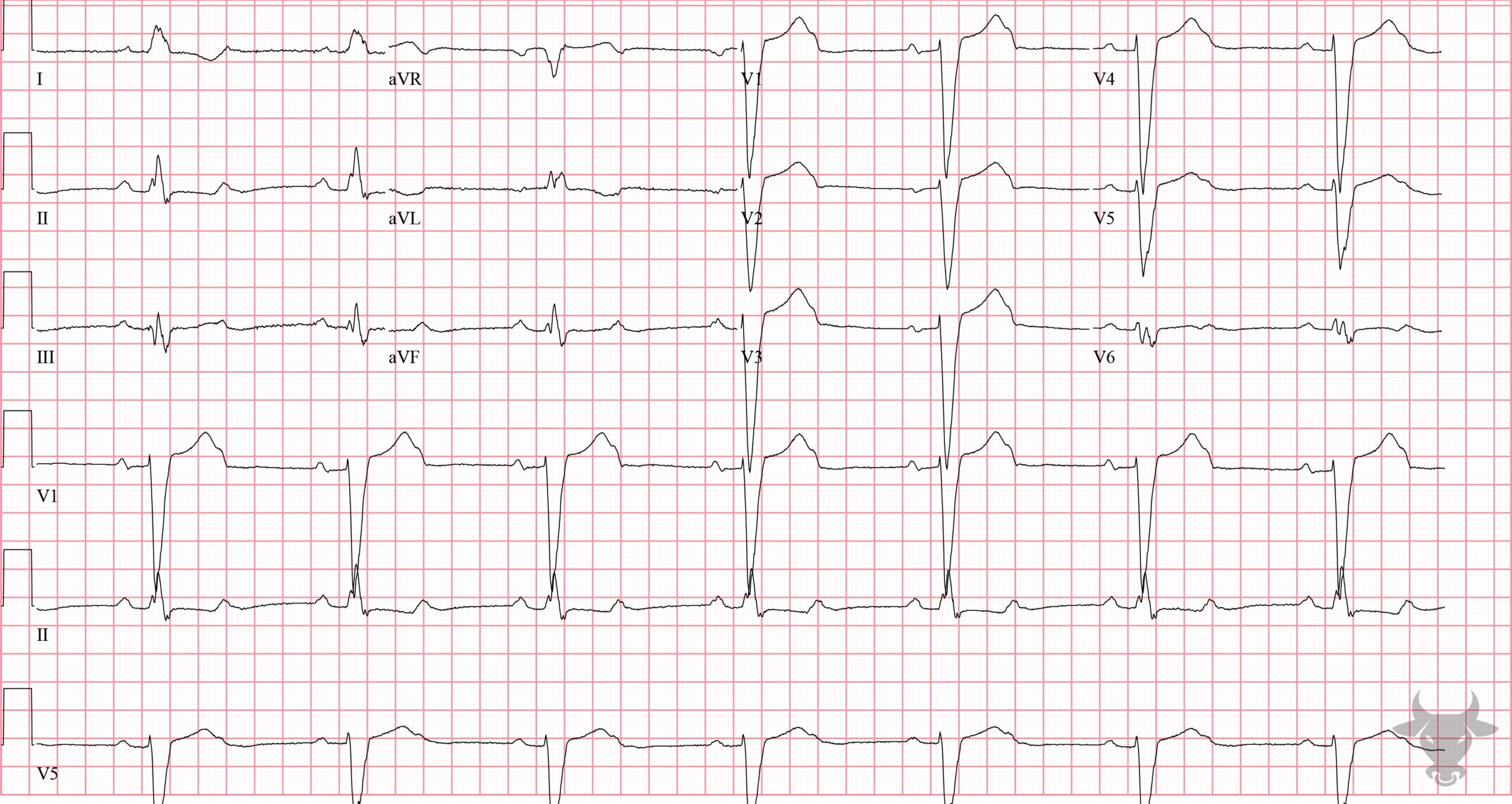
Second Degree Atrioventricular Block 2:1
Right bundle branch block, left anterior fascicular block, and 2:1 atrioventricular block. This representing Mobitz II conduction given the extent of infranodal disease. This patient was admitted for a permanent pacemaker.References
- Costa D Da, Brady WJ, Edhouse J. Bradycardias and Atrioventricular conduction block. Br Med J. 2002;324(March):535-538.
- de Pádua F, Pereirinha A, Marques N, Lopes MG, Macfarlane PW. Conduction Defects. In: Macfarlane PW, van Oosterom A, Pahlm O, Kligfield P, Janse M, Camm J, eds. Comprehensive Electrocardiology. London: Springer London; 2010:547-604.
- Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhyth. Circulation. 2019;140(8):e382-e482.
