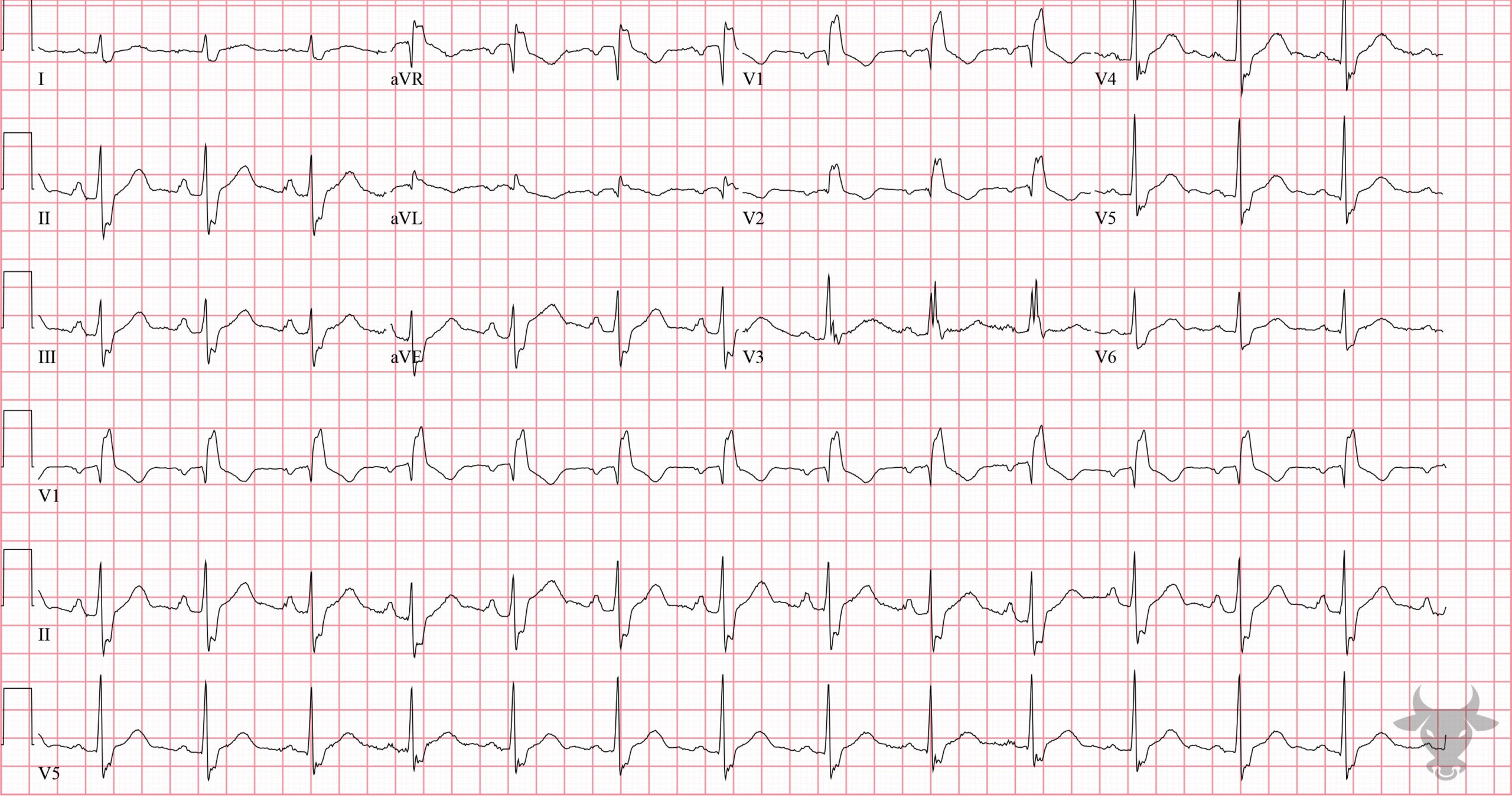
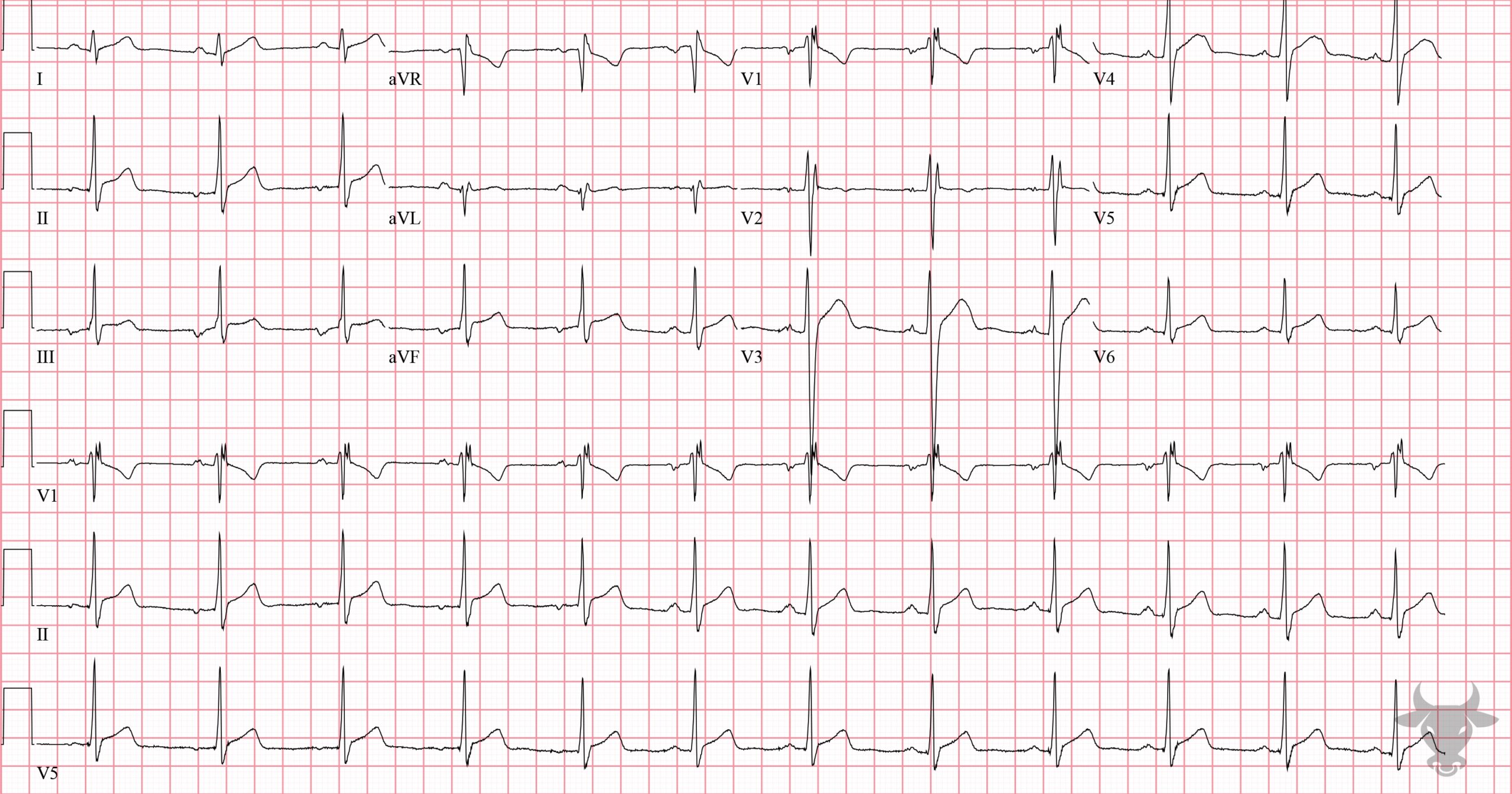
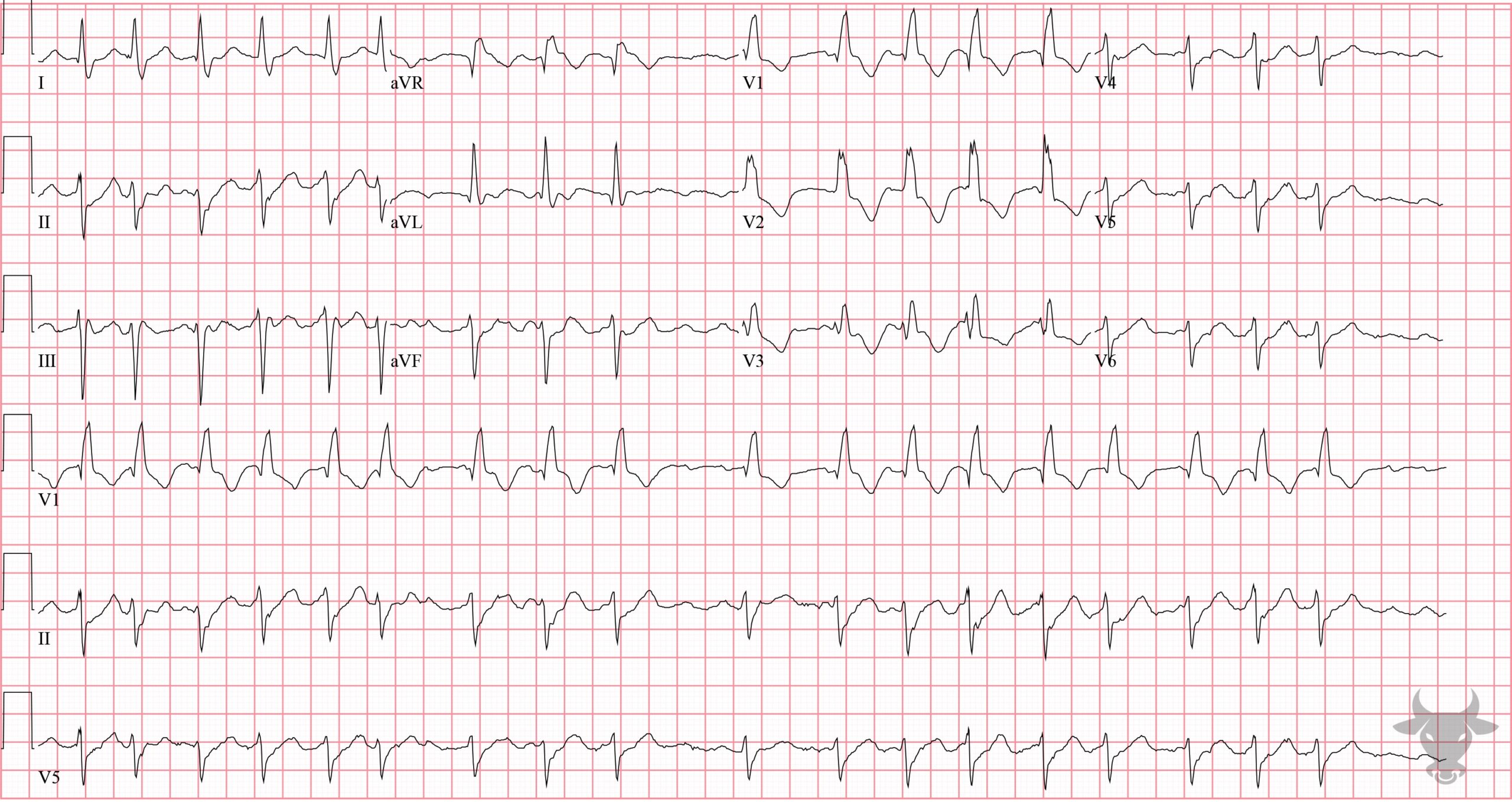
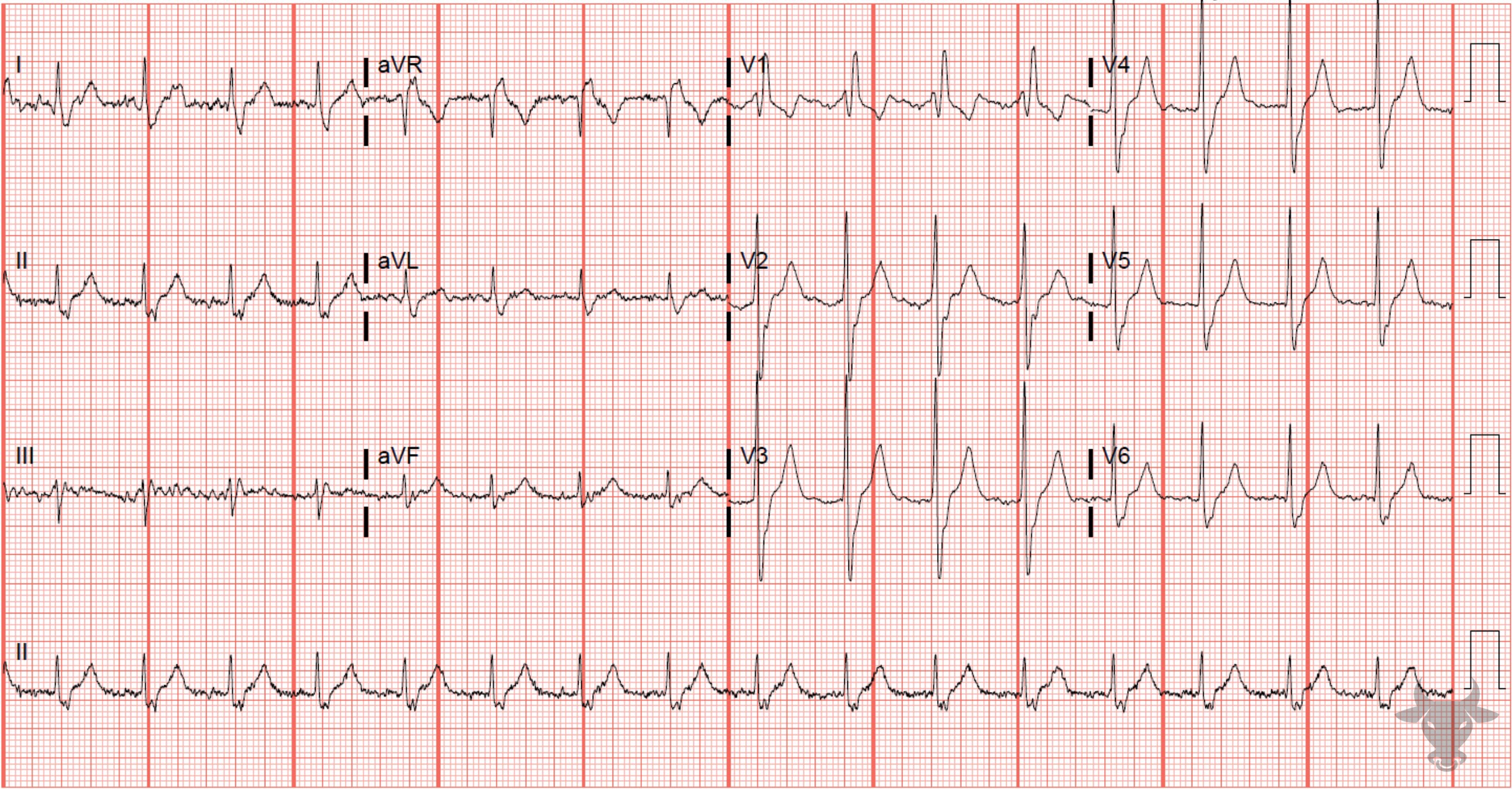
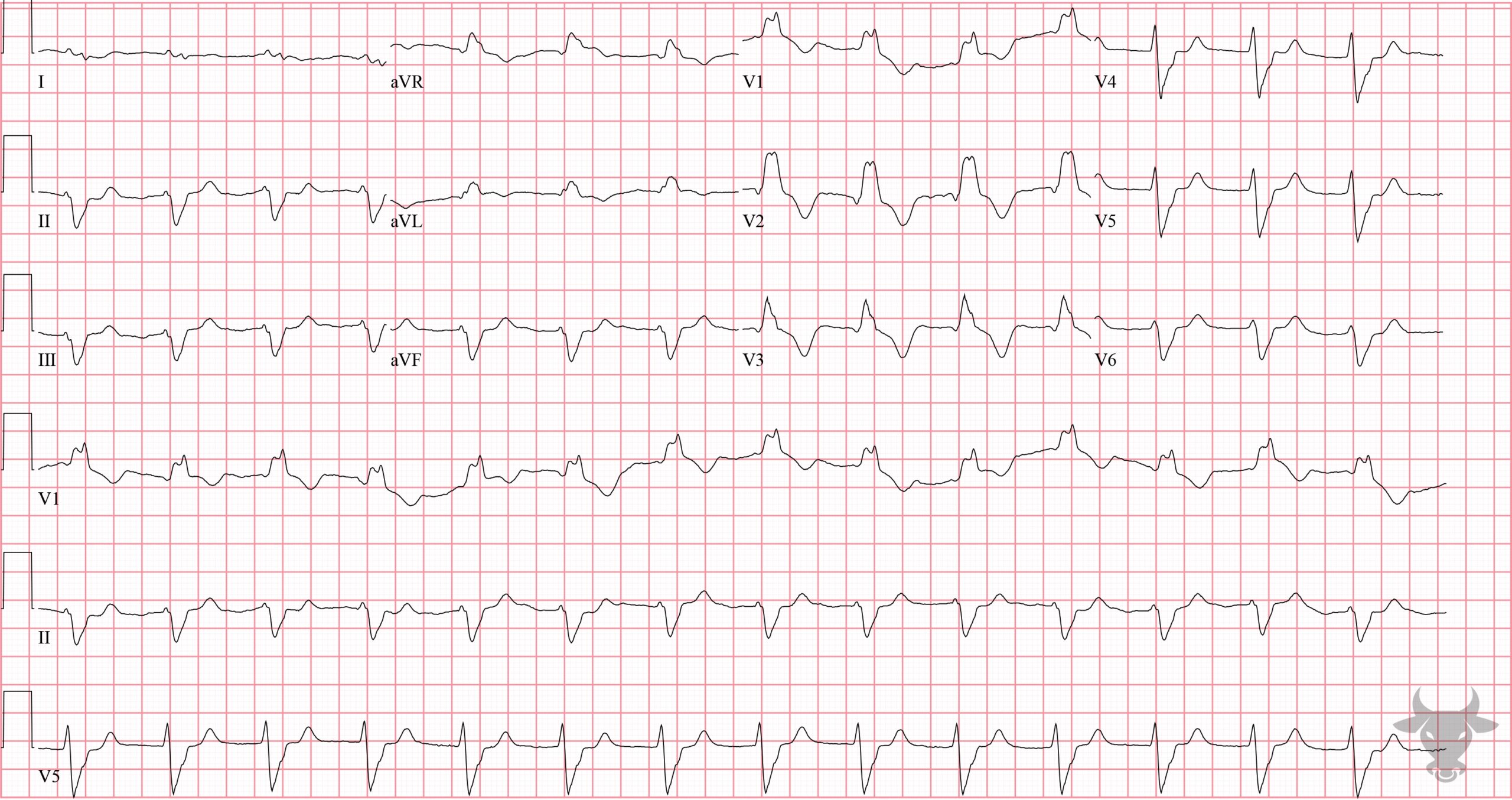
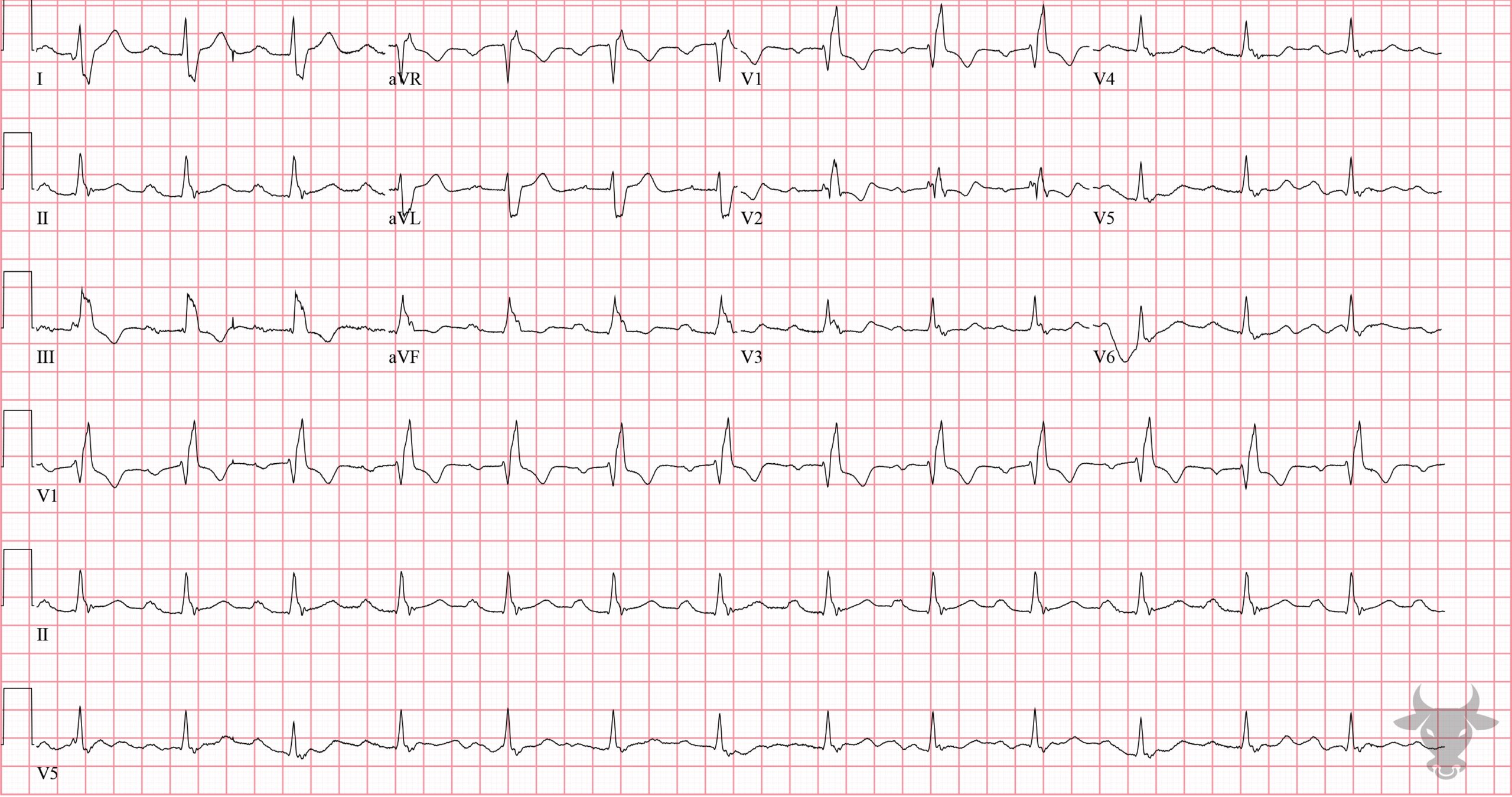
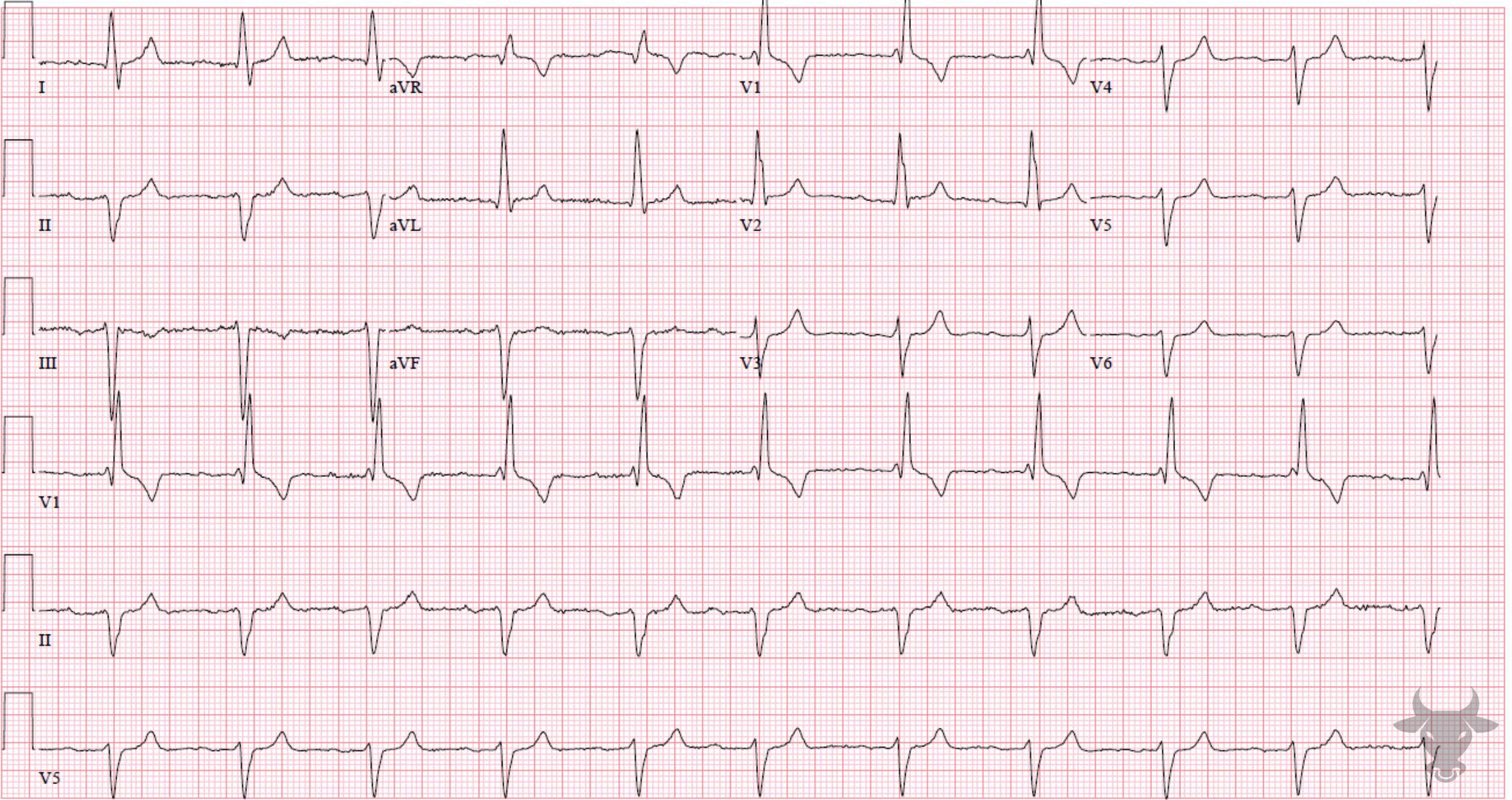
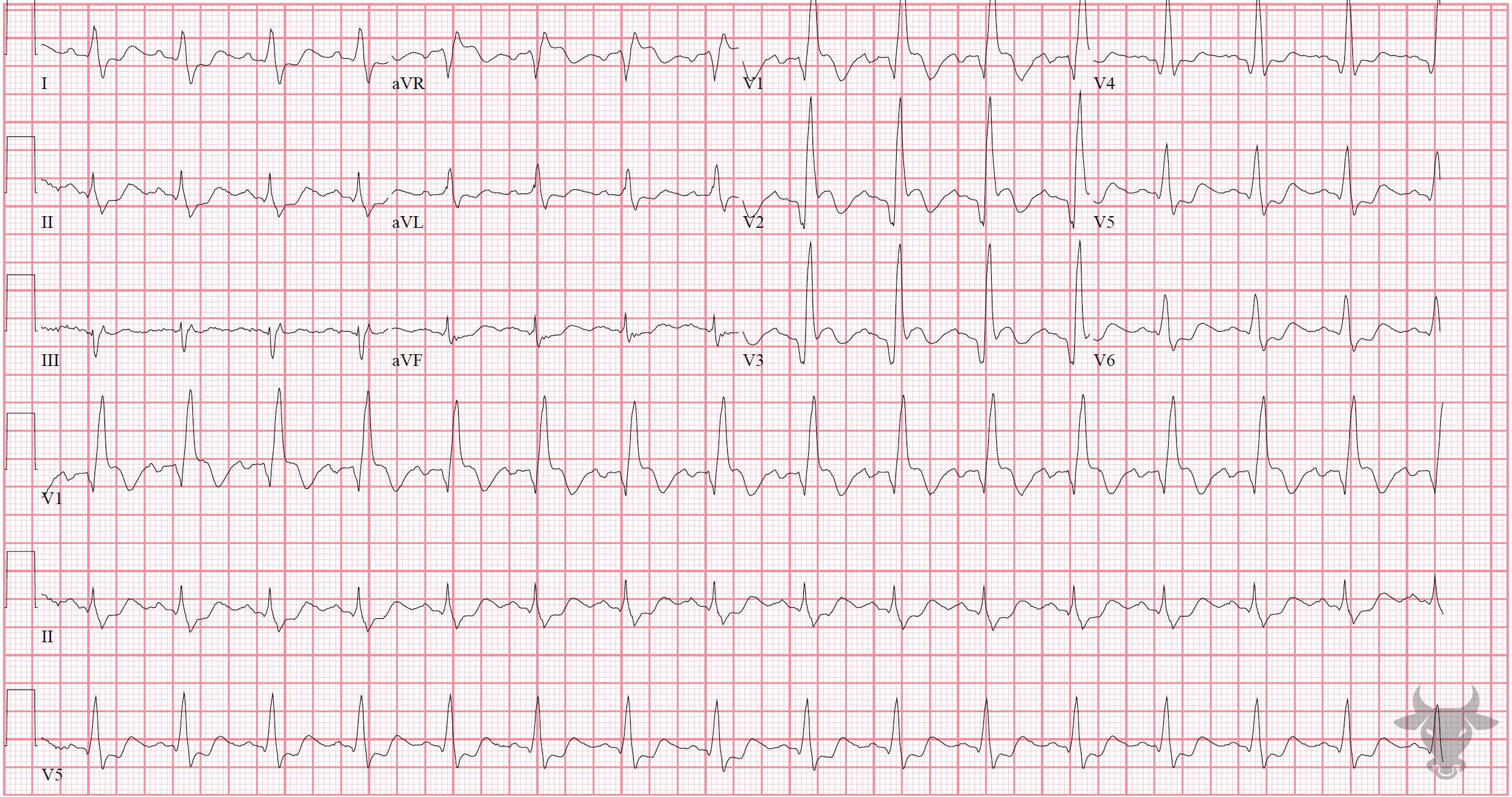
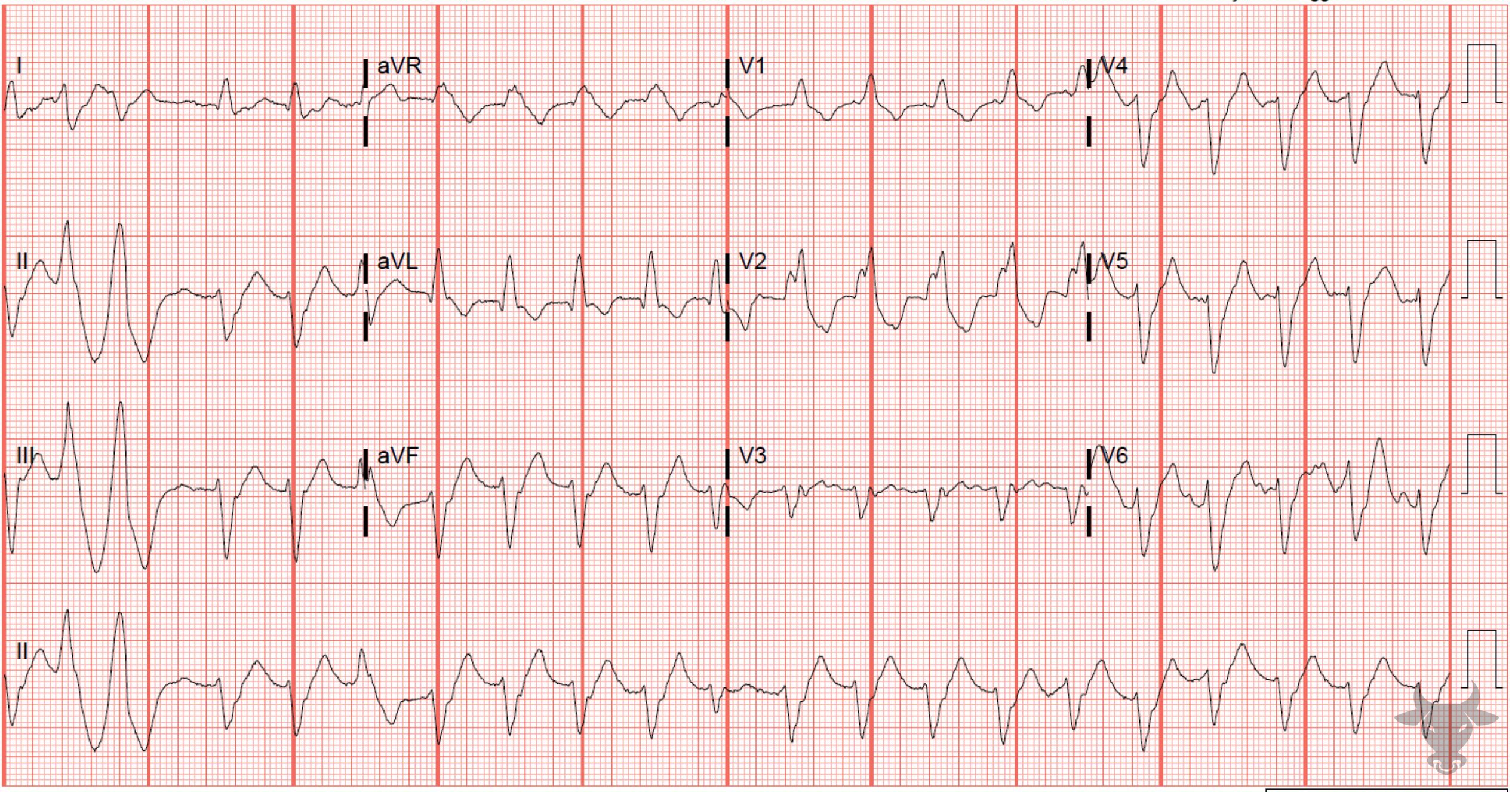
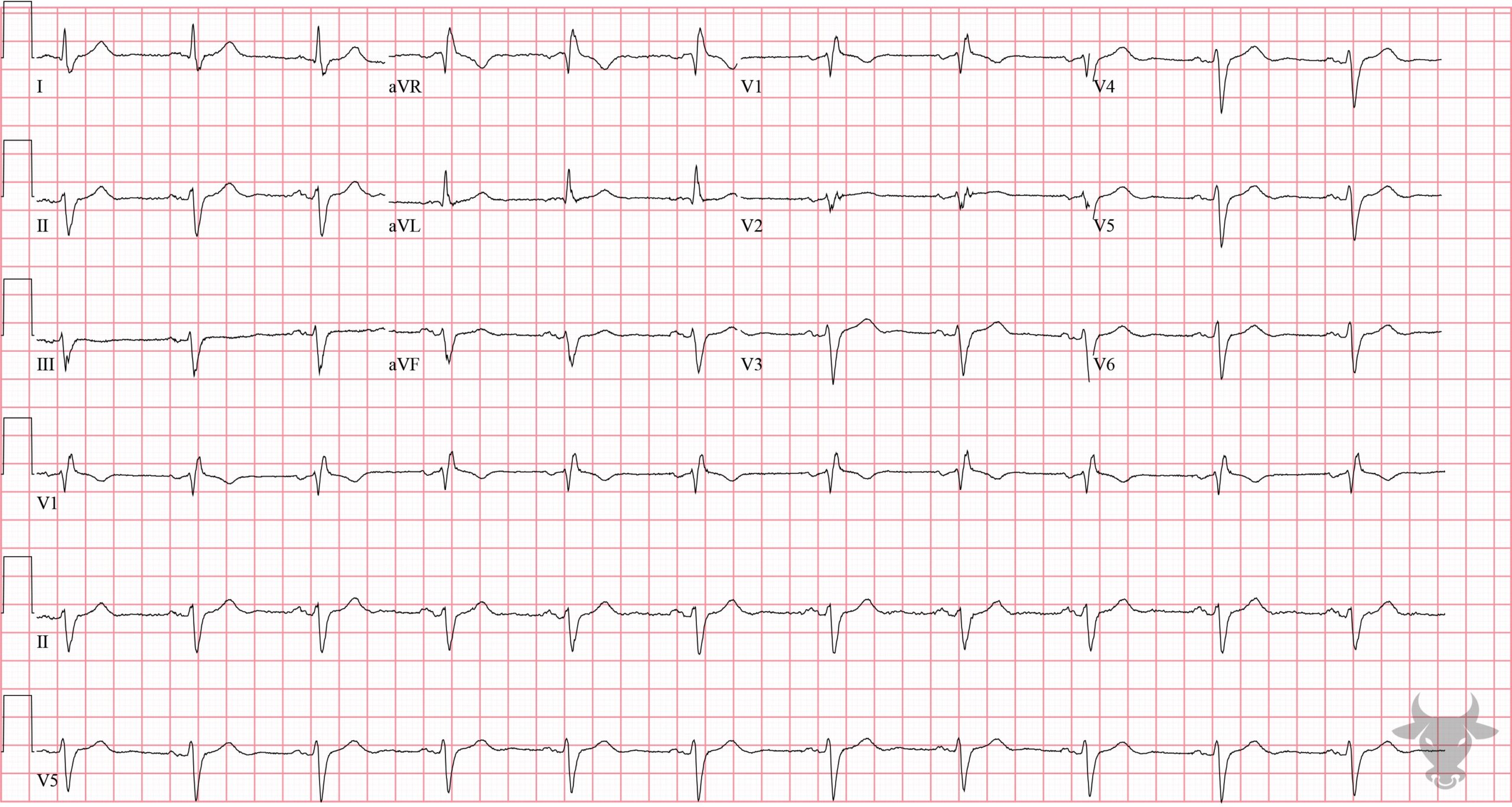
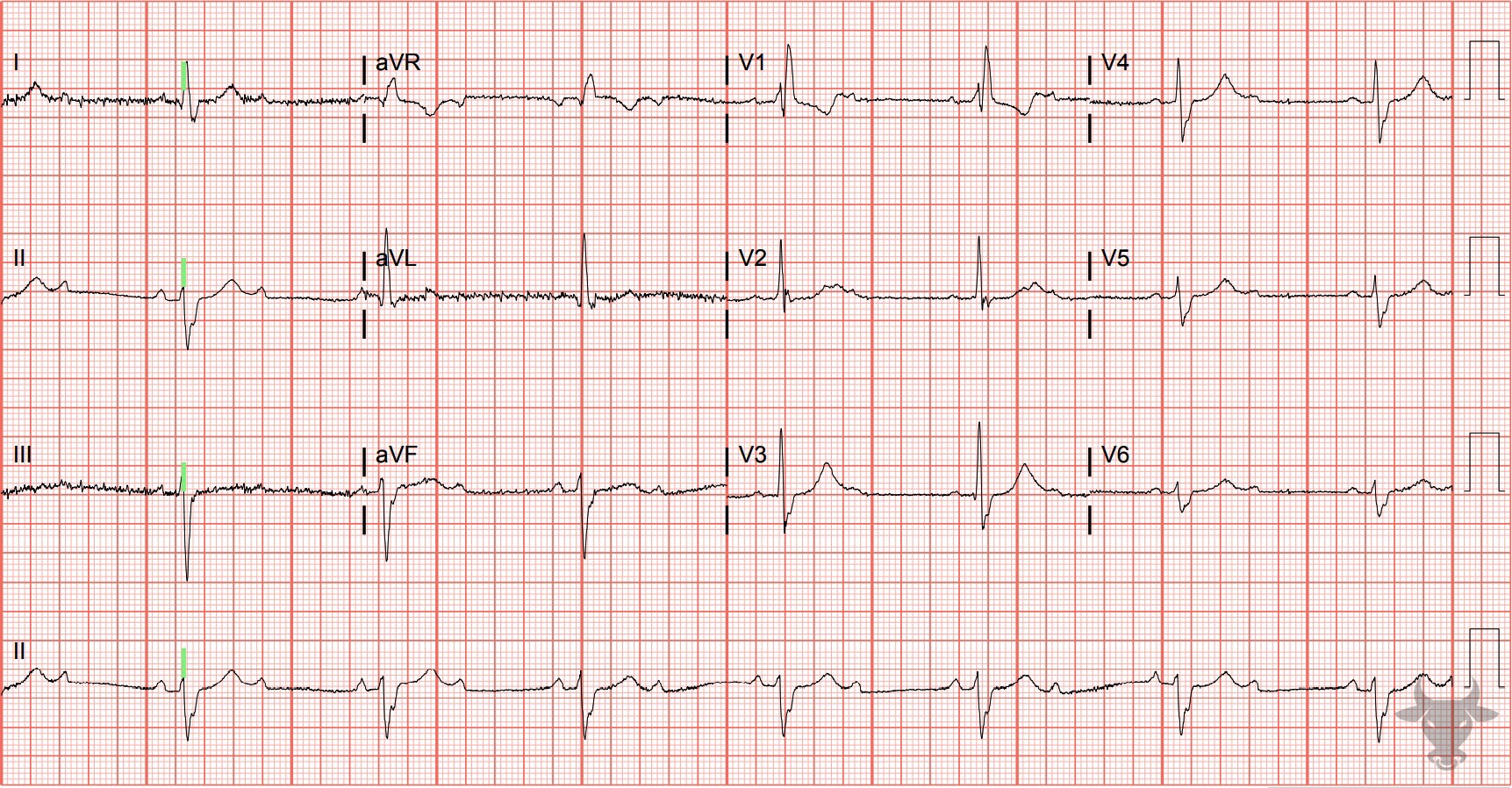
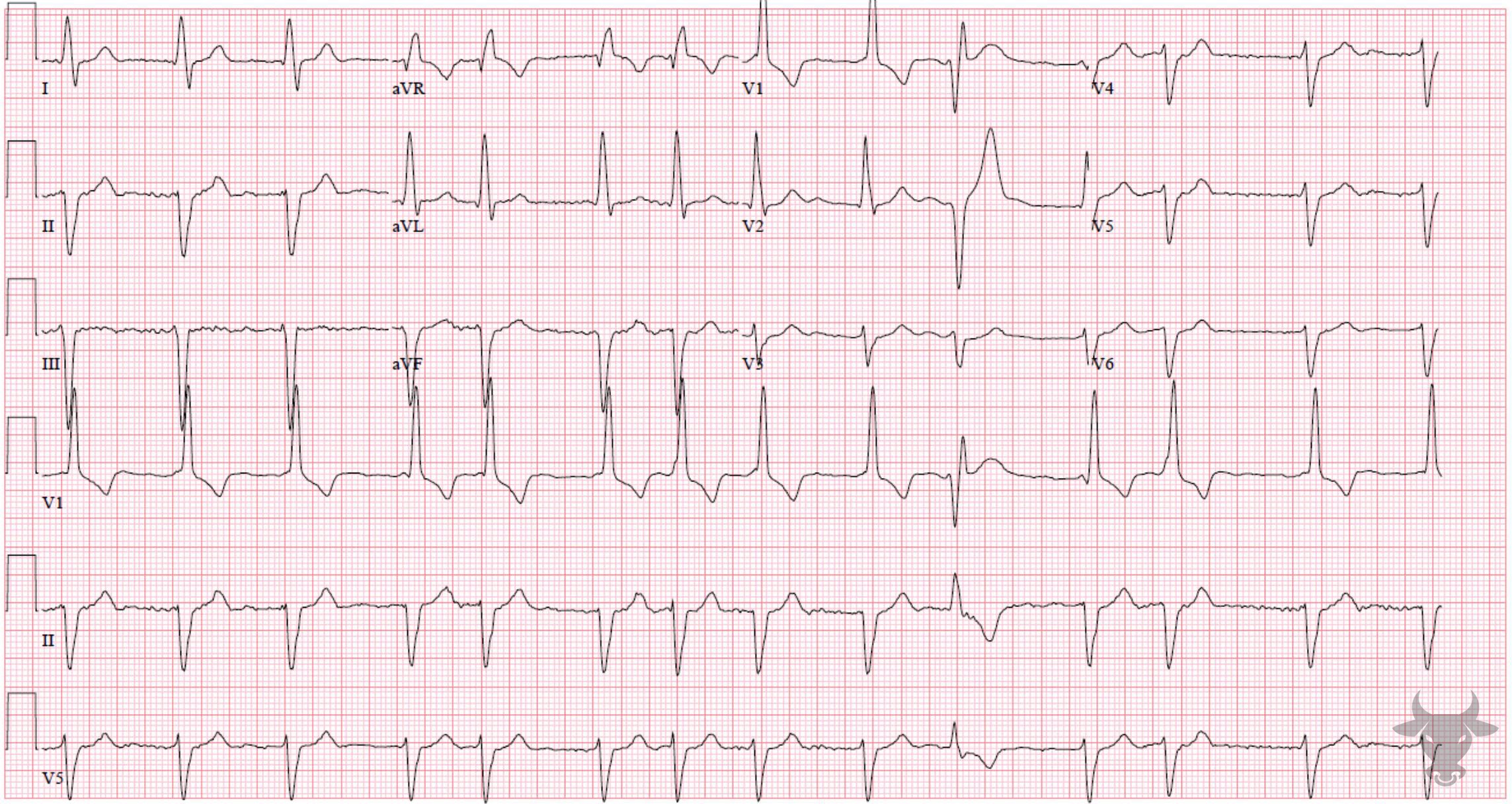
Right bundle branch block (RBBB) occurs when the right bundle no longer conducts, and the signal must pass to the right ventricle via myocyte-to-myocyte conduction. This pattern of conduction is slower than via the specialized conduction system, and results in a wide QRS complex (>120 ms). The criteria are:
- QRS > 120 ms
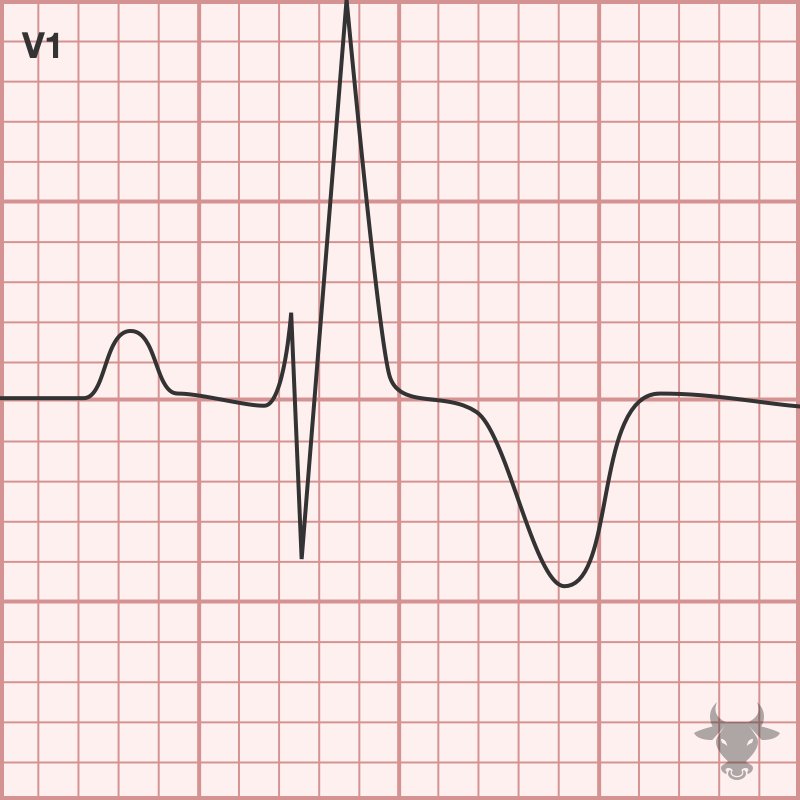
- rSR’ pattern in V1-3 (‘M-shaped’)
- Wide/slurred S wave in the lateral leads (I, aVL, V5-6)
Note that there is no right axis deviation associated with RBBB as there is a left axis deviation associated with left bundle branch block.
RBBB is common and generally not a powerful indicator of disease by itself. This is because the right bundle often has a singular blood supply as opposed to the left bundle which has a more diverse blood supply and therefore is more consistent with significant disease. However, a new RBBB in a patient with unexplained respiratory symptoms should be viewed as right ventricular outflow obstruction until proven otherwise. RBBB can be caused by right ventricular hypertrophy/cor pulmonale, pulmonary embolism, ischemic heart disease, rheumatic heart disease, myocarditis or cardiomyopathy, degenerative disease of the conduction system, or congenital heart disease (e.g., atrial septal defect).
Expected repolarization abnormalities in the setting of RBBB include T wave inversions in V1-3 and slight discordant ST depressions. ST elevation in these leads is never normal; even slight ST elevations in V1-3 may represent STEMI.
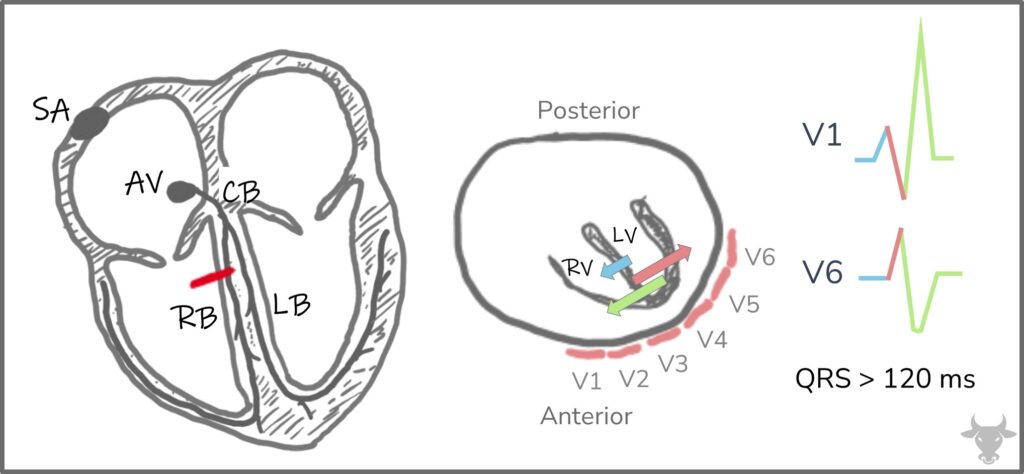
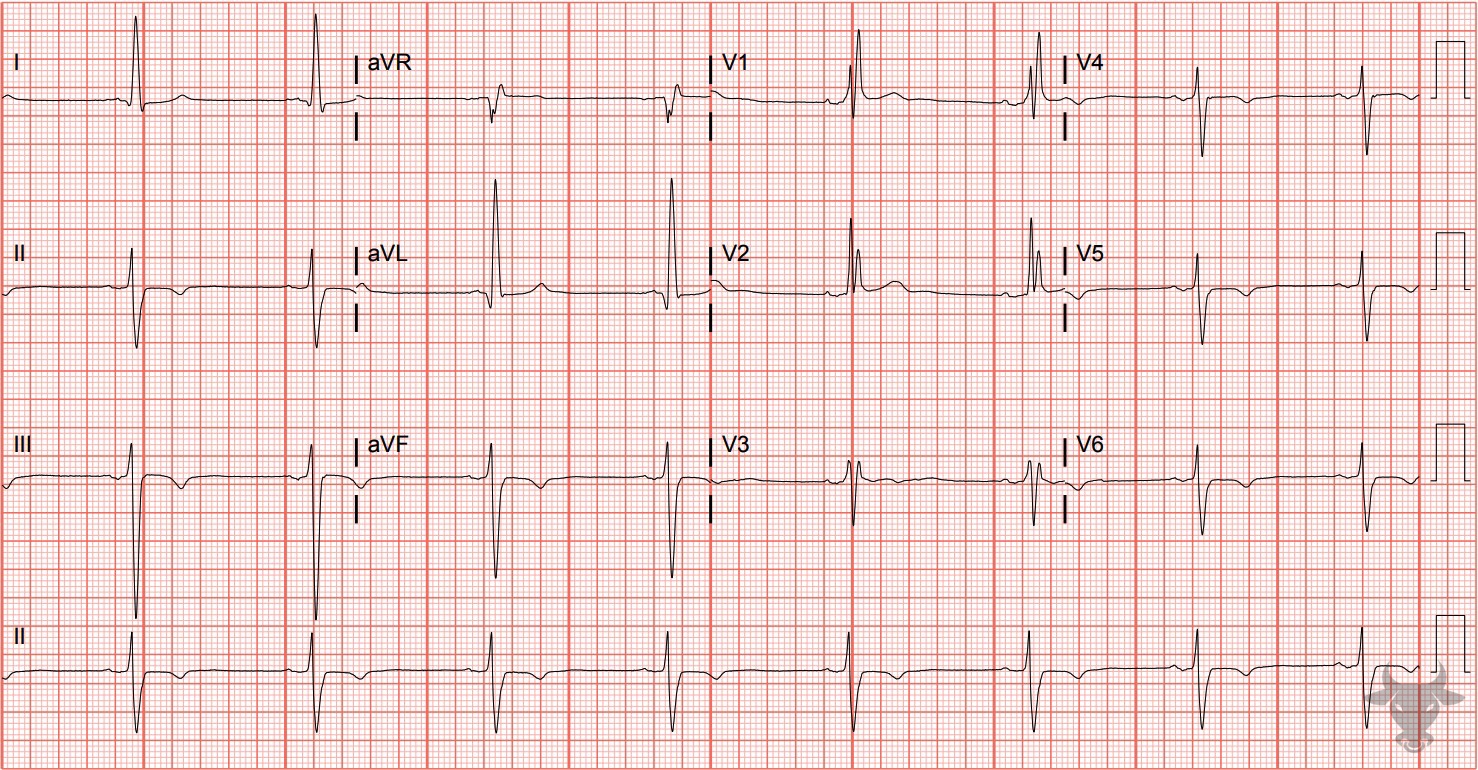
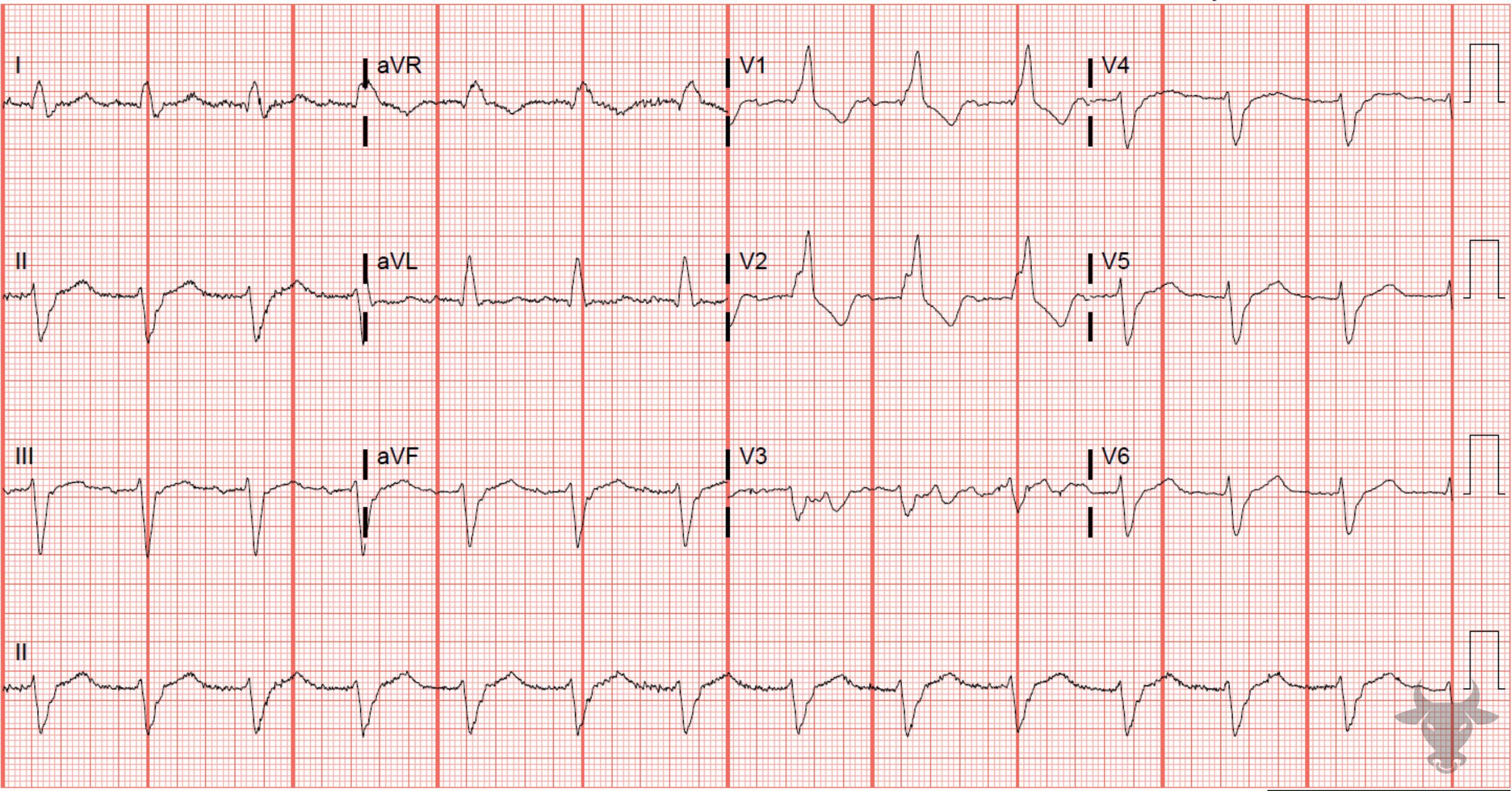
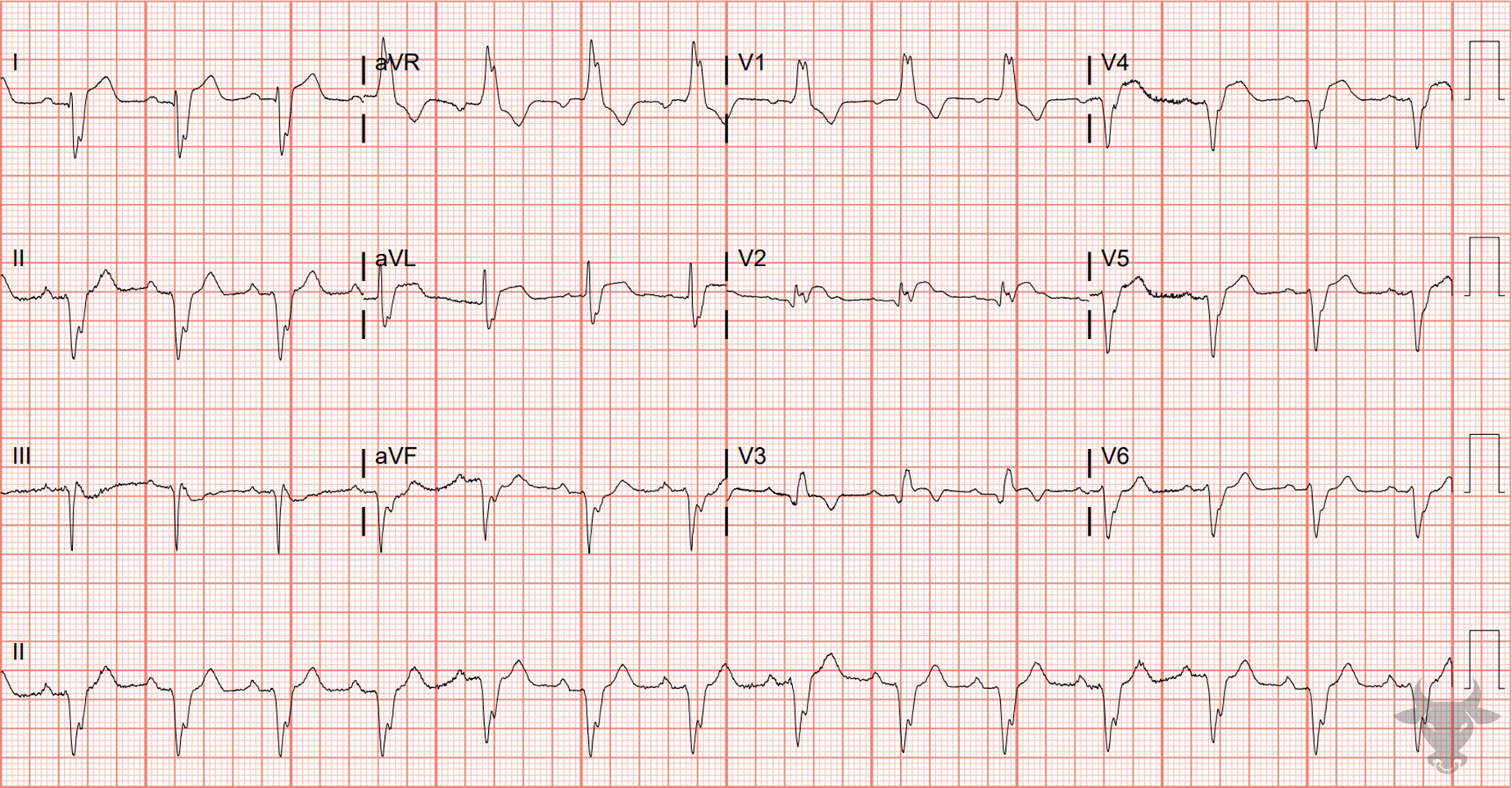
Direction of depolarization in right bundle branch block. The septum first depolarizes from left to right (blue arrow), followed by left ventricular depolarization (pink arrow), and, finally, right ventricular depolarization (green arrow). The result is an rSR’ pattern in V1, and a wide S wave in the lateral leads (I, aVL, V5, V6). SA, sinoatrial node; AV, atrioventricular node; RB, right bundle; LB, left bundle; CB, common bundle; RV, right ventricle; LV, left ventricle; red dash represents a block of the right bundle.