First degree blocks are characterized by a prolonged PR interval (greater than 200 ms) and are usually seen it active, healthy patients without heart disease. It usually represents high vagal tone within the atrioventricular node itself and is unlikely to progress to complete heart block; however, when accompanied by preexisting conduction disease (e.g. right bundle branch block, left bundle branch block, or bifascicular block) it can indicate infranodal conduction disease.
First Degree Atrioventricular Block
Examples
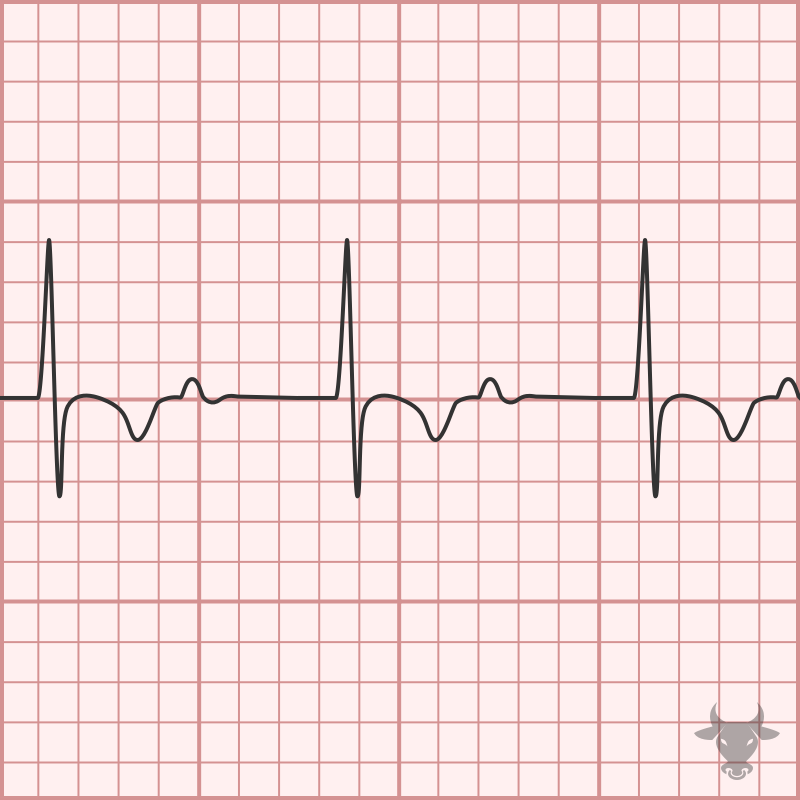
First Degree Atrioventricular Block
Prolonged PR interval representing first degree atrioventricular block.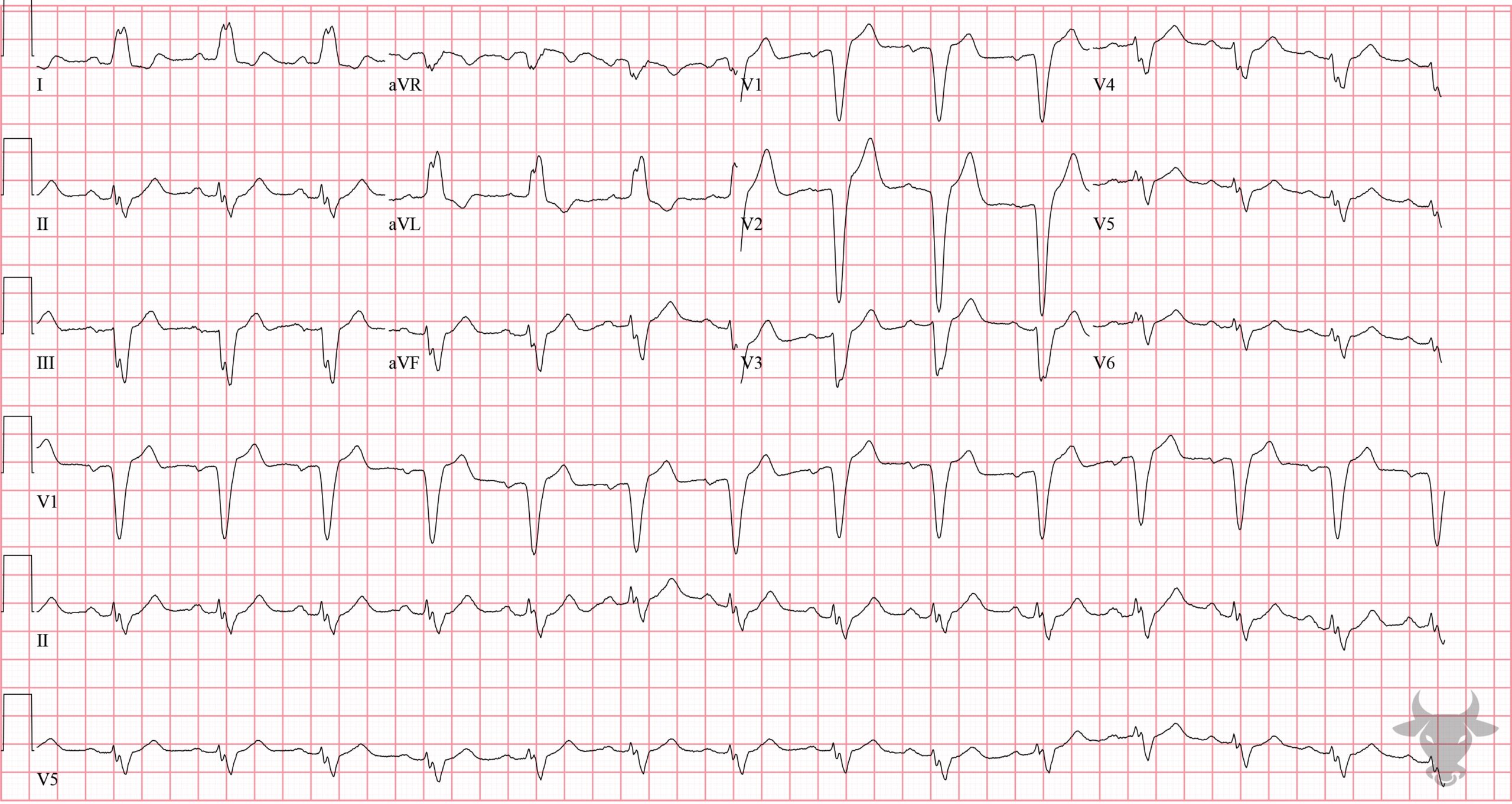
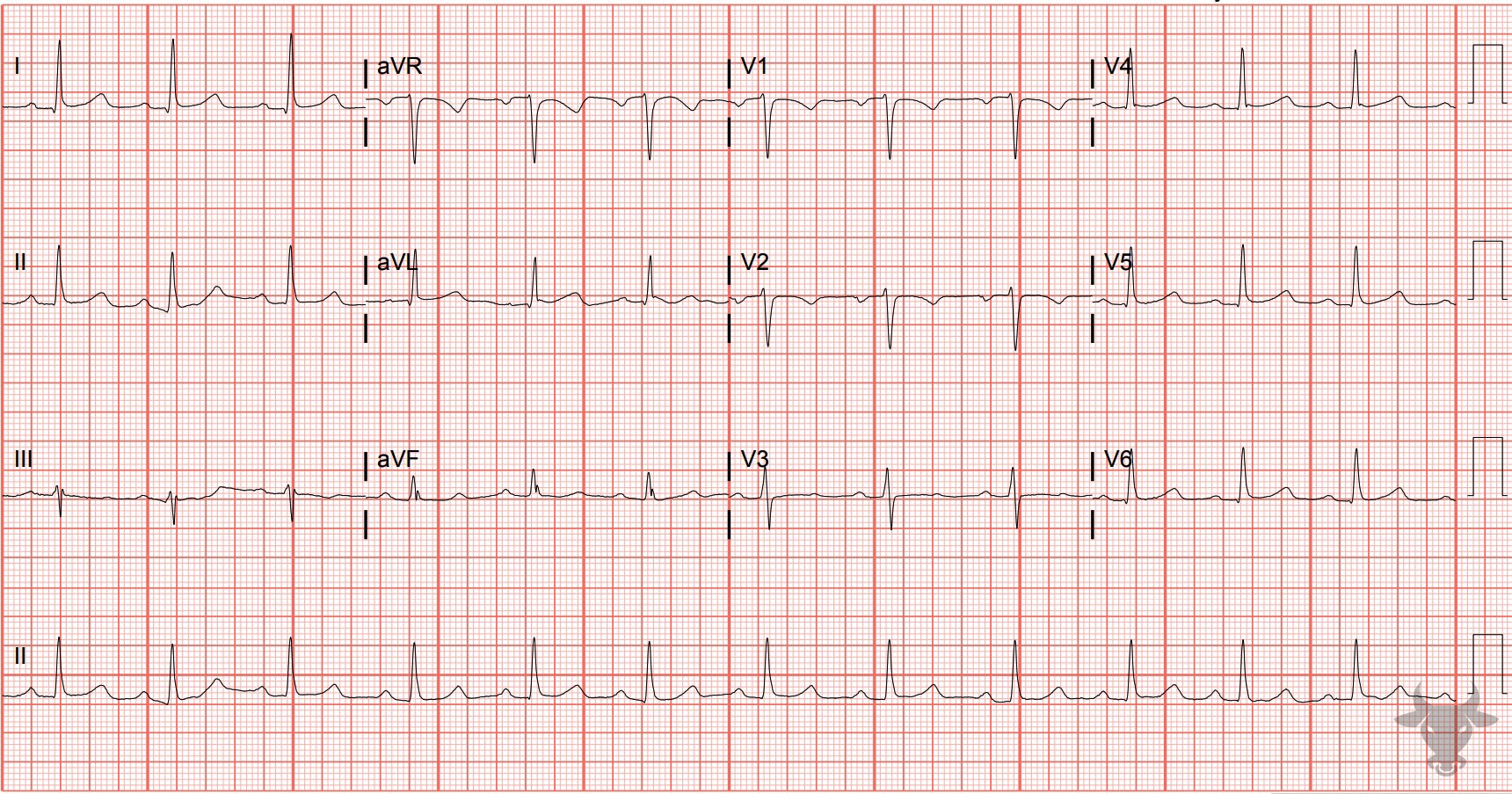
Left Bundle Branch Block
The PR interval is borderline at 200 msec. When a left bundle branch block is accompanied with a first degree atrioventricular block, this suggests trifascicular disease. This patient subsequently went into complete heart block and lost consciousness.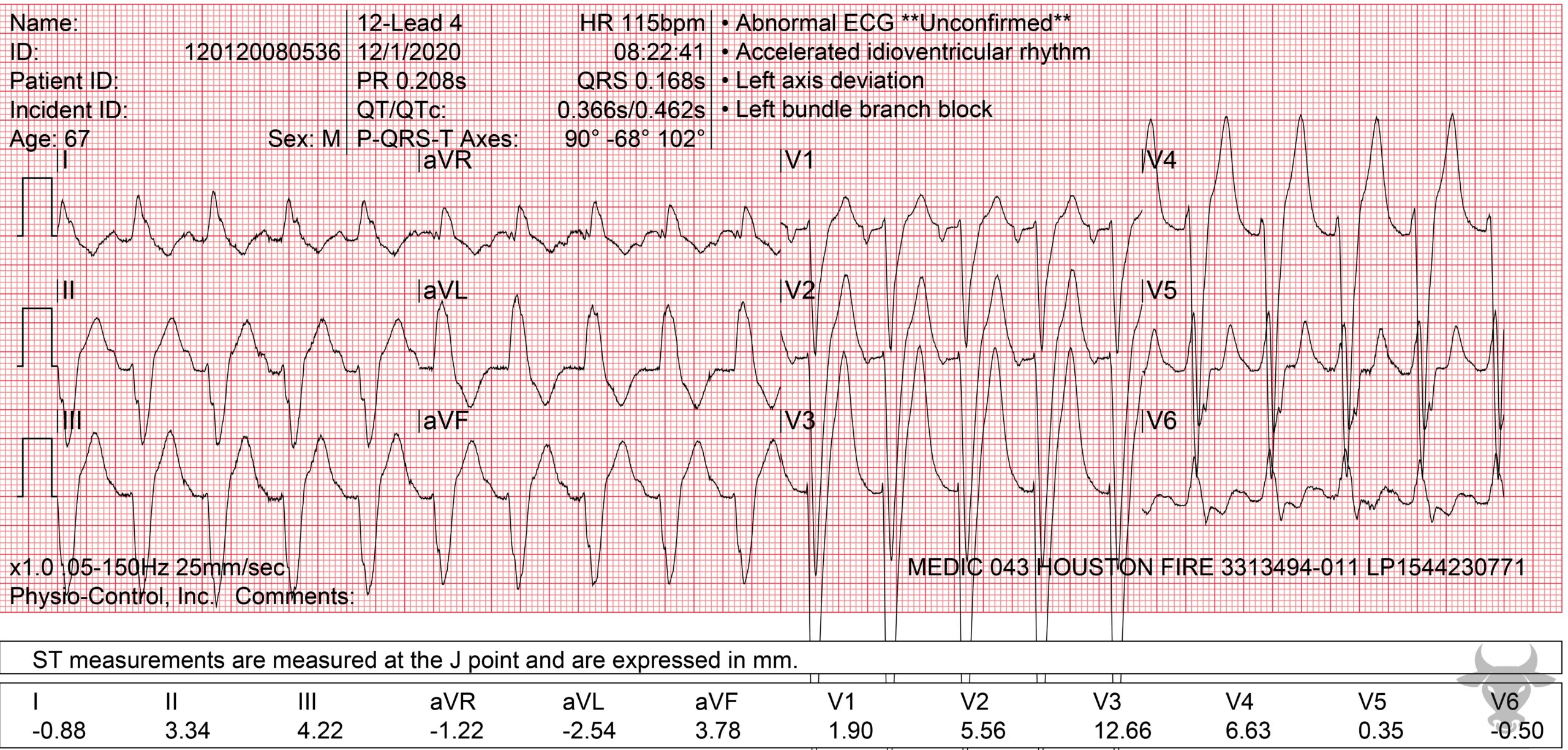
Left Bundle Branch Block
When associated with a first degree atrioventricular block, a left bundle branch block can be misinterpreted as ventricular tachycardia, or, in this case, an accelerated idioventricular rhythm. The P wave is buried by the preceding T wave, masking the atrial activity. This patient was in sinus tachycardia (P waves are most clearly seen in V1).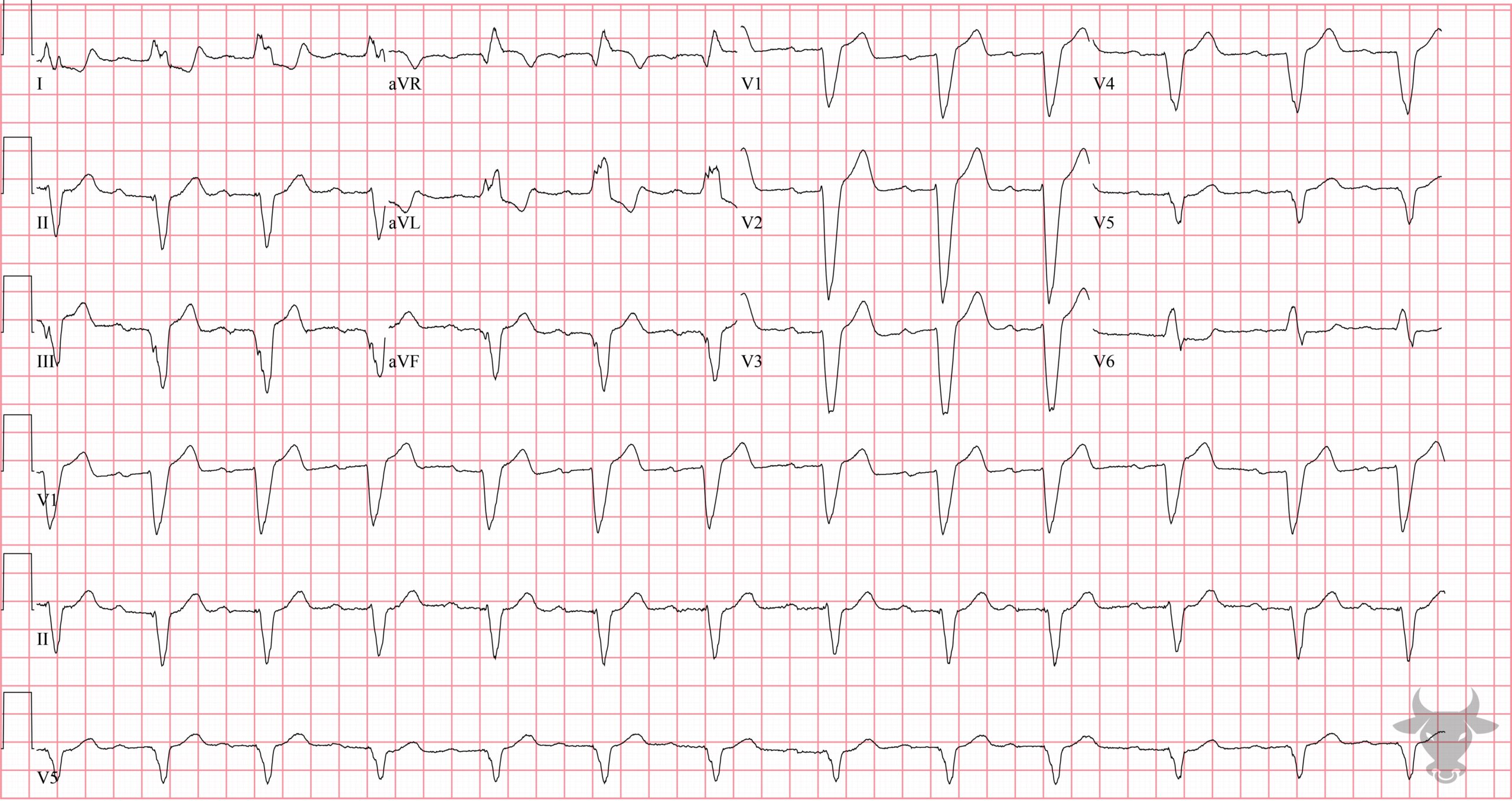
Left Bundle Branch Block
While not classically referred to as a "trifascicular block," left bundle branch blocks indicate the failure of two fascicles - the left anterior and posterior fascicles - and, when associated with a first degree atrioventricular block (i.e., prolonged PR interval), likely represents trifascicular disease. This patient presented with syncope and subsequently received a permanent pacemaker after telemetry revealed intermittent high-gade atrioventricular block while inpatient.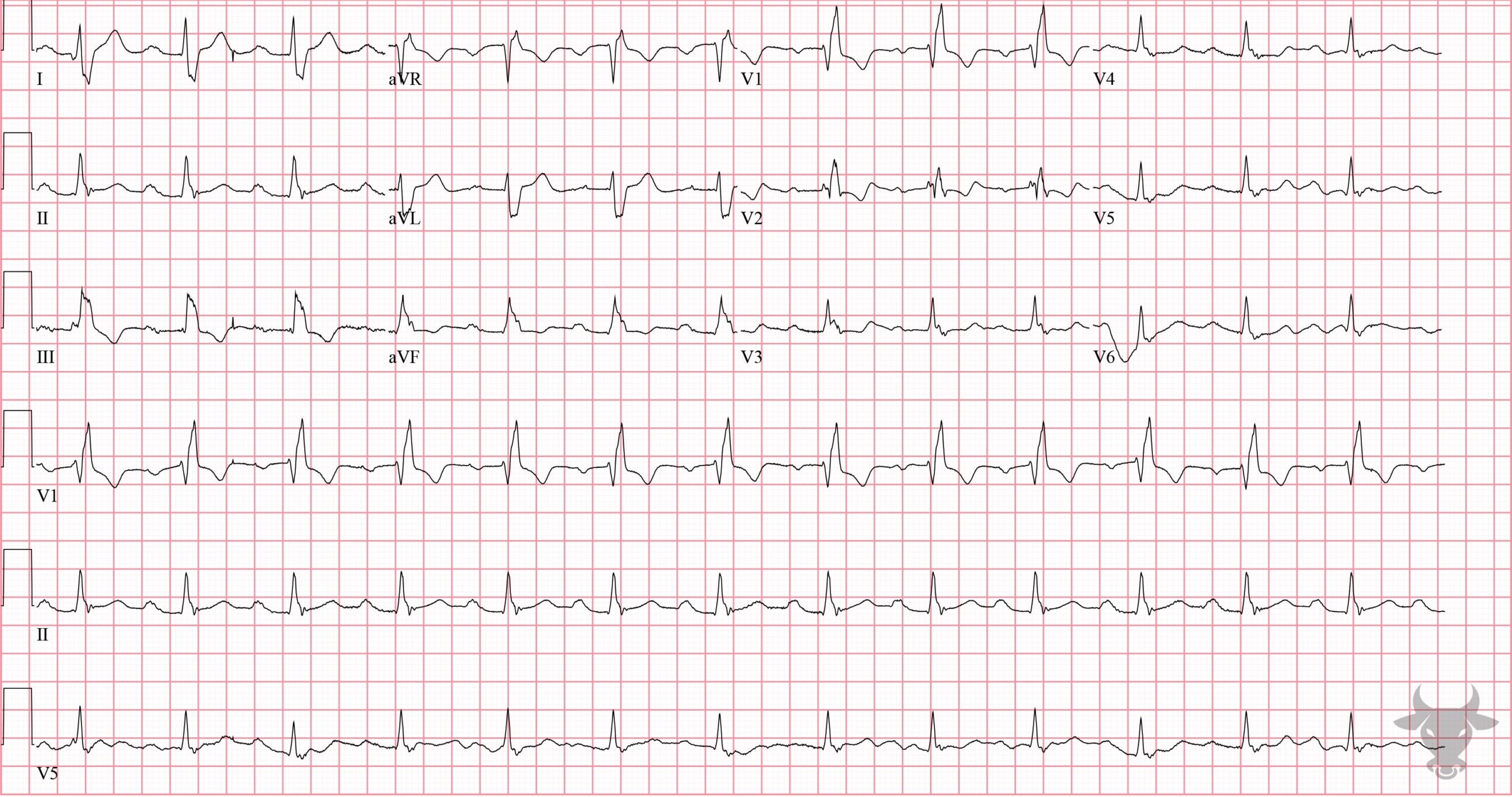
Right Bundle Branch Block
Classic RBBB pattern with first degree atrioventricular block in a patient with right heart failure from obesity hypoventilation syndrome.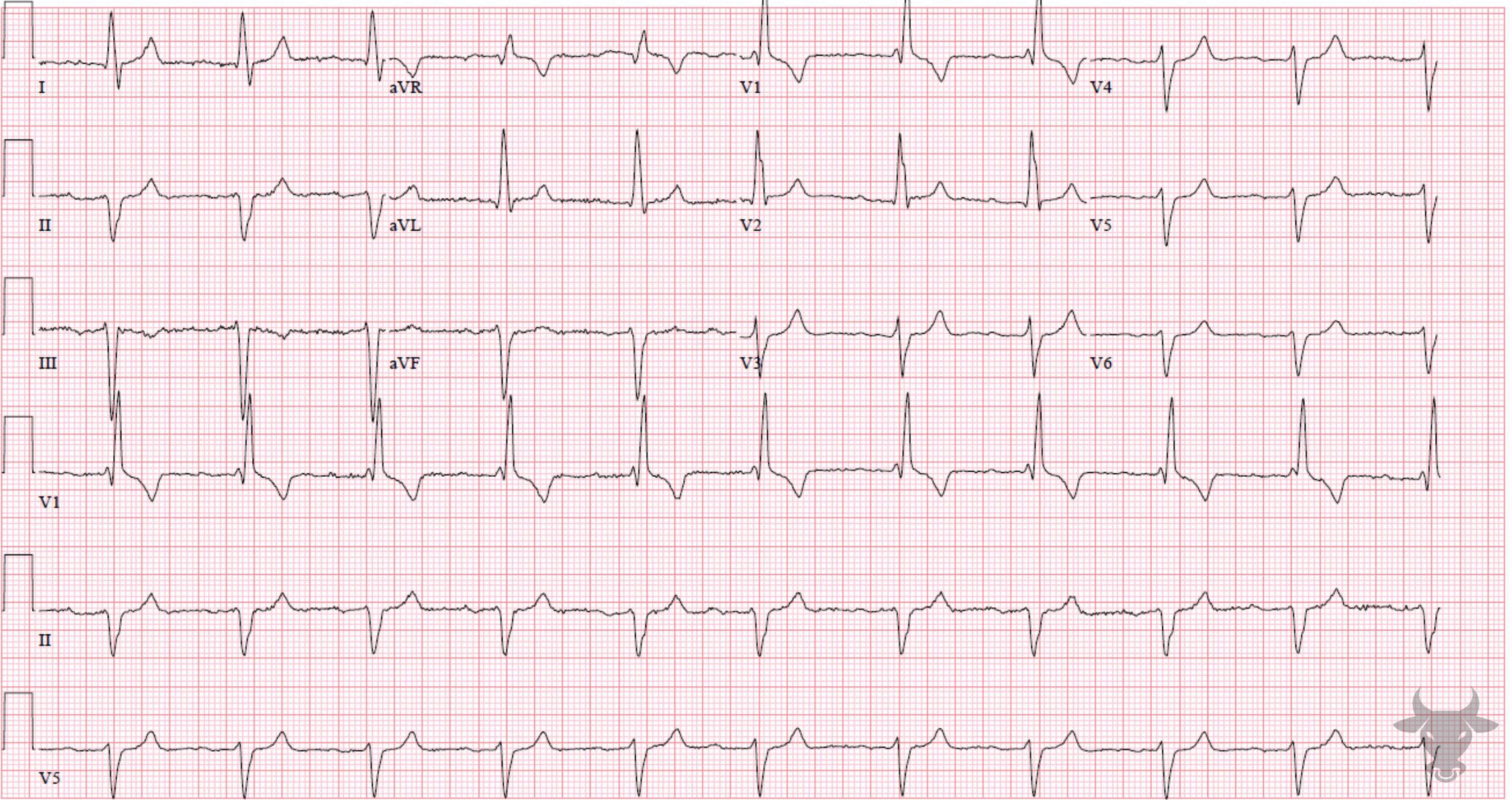
Trifascicular Block
Right bundle branch block and left anterior fascicular block with a prolonged PR interval. This represents disease of all three fascicles, so called "trifascicular block."References
- Surawicz B, Childers R, Deal BJ, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2009;53(11):976-81.
- Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. J Am Coll Cardiol. 2019;74(7):932-987.
