When two of three fascicles are blocked, it is termed bifascicular block. While a left bundle branch block (LBBB) technically involves disruption of two fascicles, this term is typically reserved for the combination of a right bundle branch block (RBBB) with a left anterior fascicular block (LAFB) or a left posterior fascicular block (LPFB). Causes include ischemic heart disease (40-60% cases), hypertension (20-25%), aortic stenosis, anterior myocardial infarction (occurs acutely in 5-7%), primary degenerative disease of the conducting system (Lenegre’s/Lev’s disease), congenital heart disease, and hyperkalemia. Recall that RBBB is not normally associated with axis deviation (unlike LBBB); therefore, right axis deviation in the setting of RBBB is most likely explained by the presence of a LPFB. In the same way that a LAFB causes left axis deviation, a LPFB causes a right axis deviation. Bifascicular blocks are clinically relevant because they can progress to complete heart block. In patients with syncope, one early study suggests a 17% cumulative incidence of complete atrioventricular block within five years.
Bifascicular Block
Examples
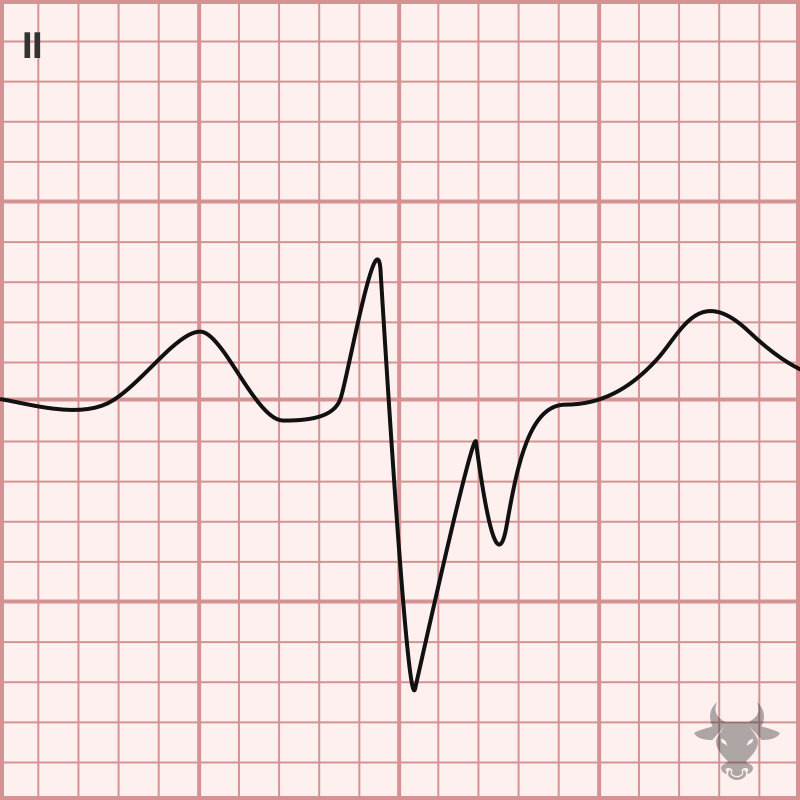
Right Bundle Branch Block & Left Posterior Fascicular Block
Right bundle branch blocks do not typically cause an axis deviation because the right ventricle does not have enough myocardium to cause an axis shift (as opposed to a left bundle branch block). When a right axis deviation accompanies a right bundle branch block, there is often an associated left posterior fascicular block, as with this case.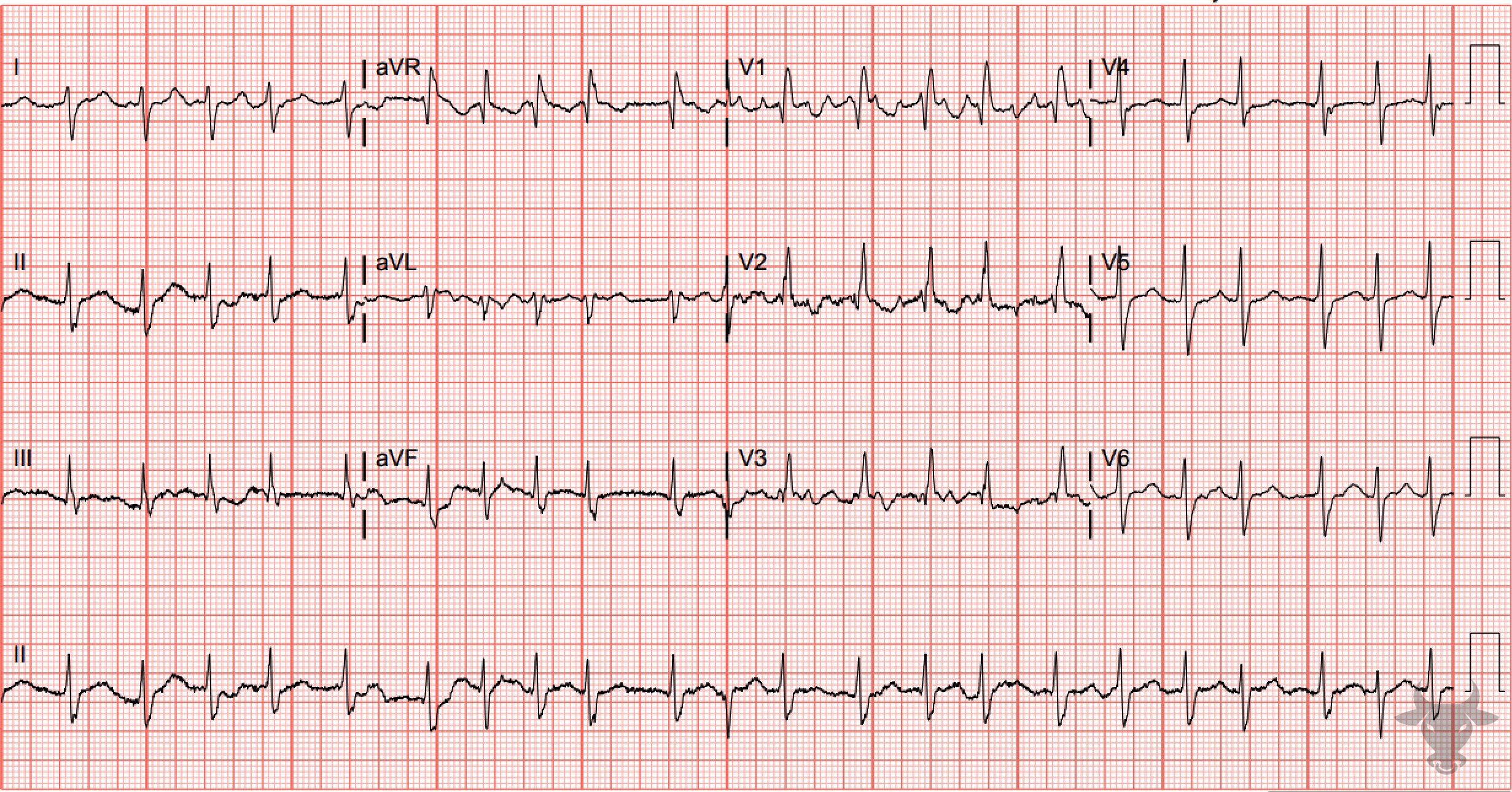
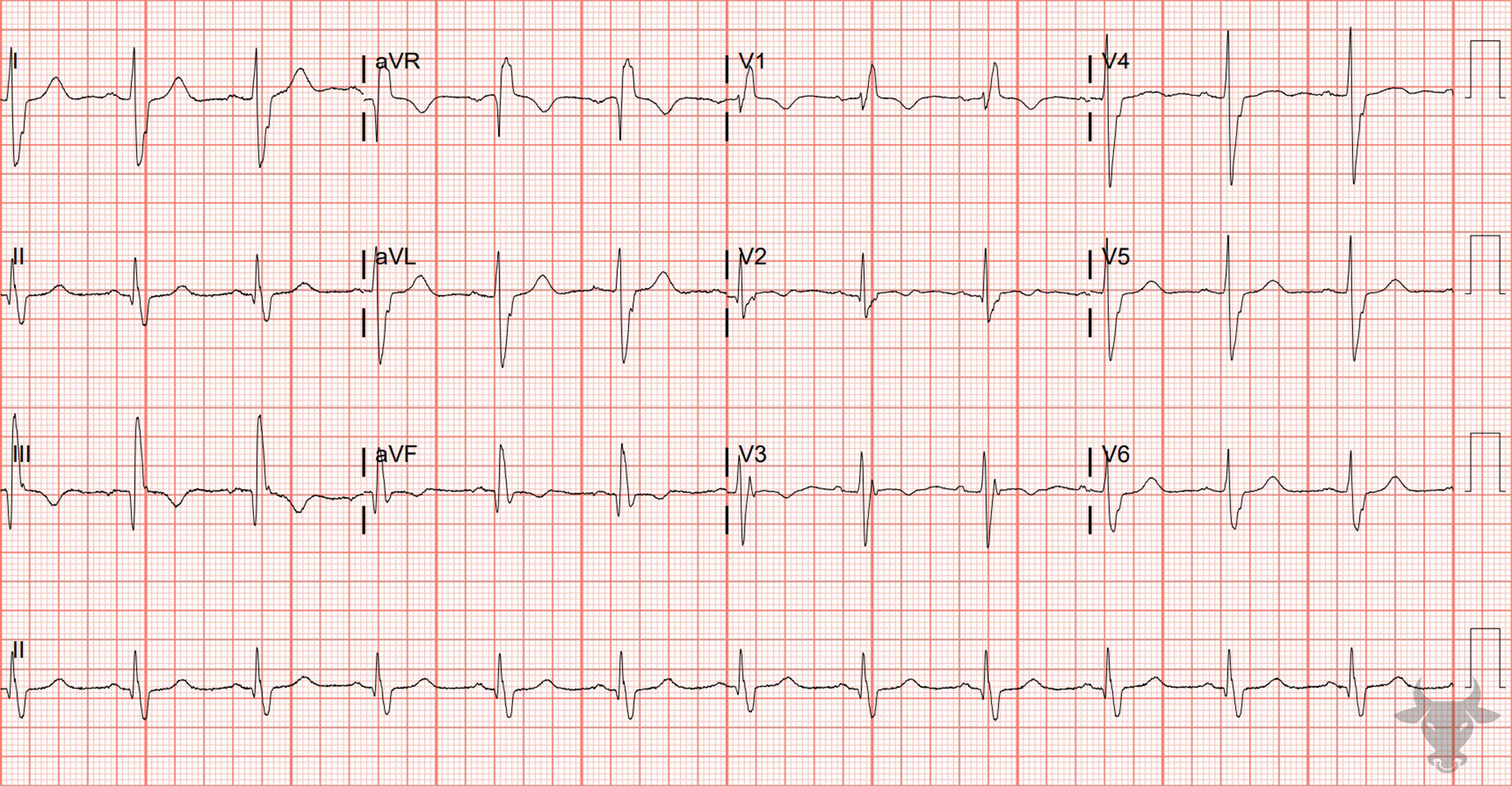
Right Bundle Branch Block & Left Posterior Fascicular Block
The rhythm is irregularly irregular as a result of atrial fibrillation. There is a right bundle branch block and a left posterior fascicular block.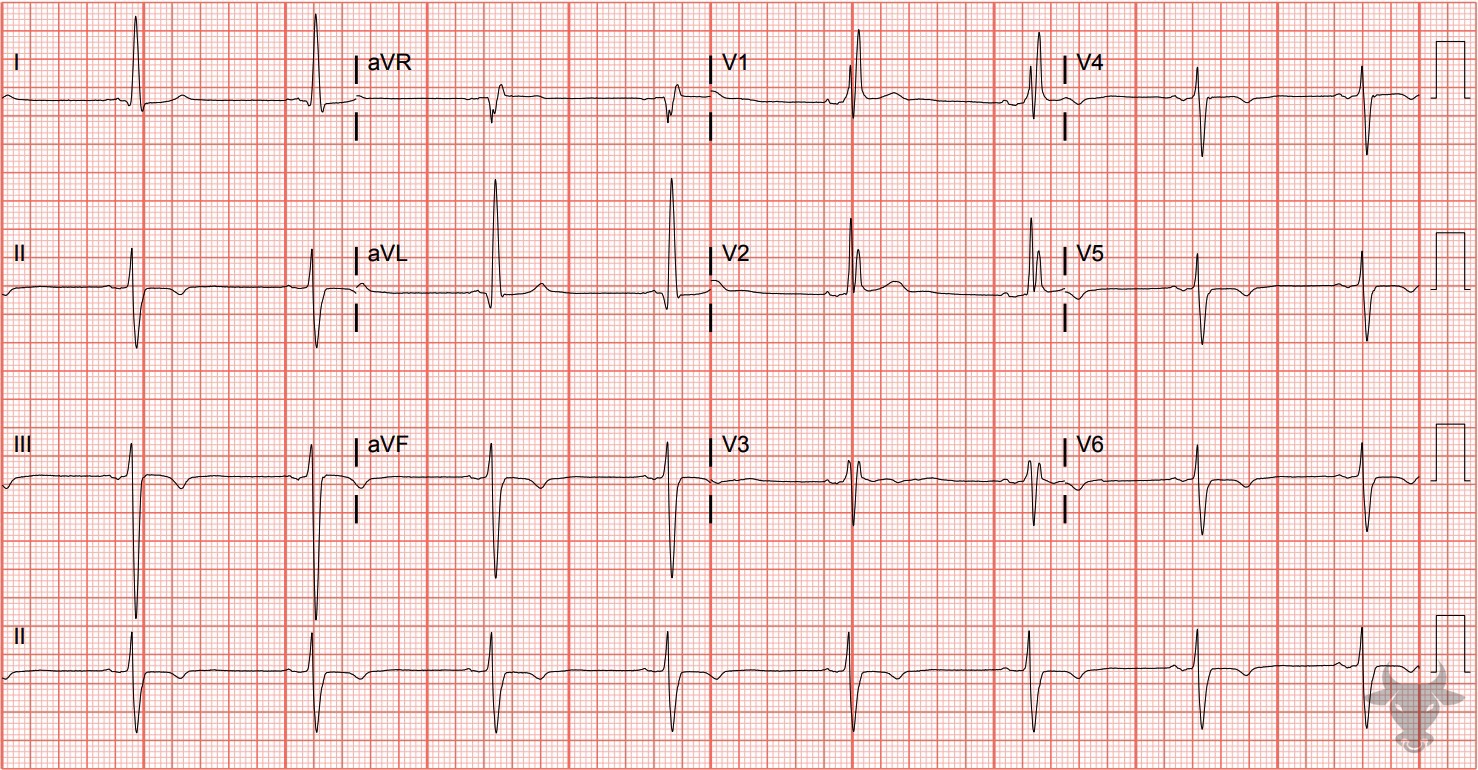
Right Bundle Branch Block & Left Anterior Fascicular Block
There is a right bundle branch block and a left anterior fascicular block.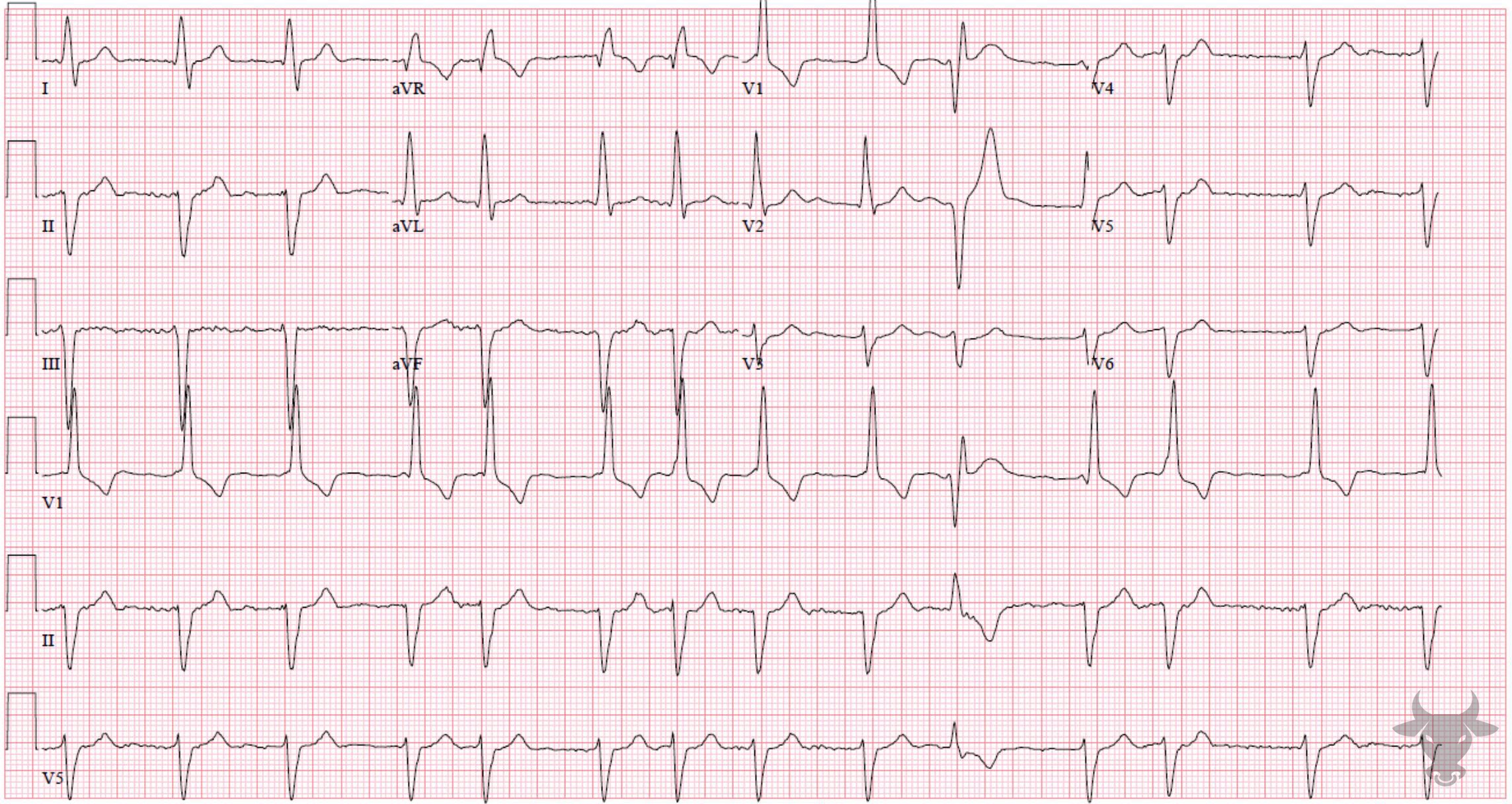
Right Bundle Branch Block & Left Anterior Fascicular Block
Right bundle branch block and left anterior fascicular block with atrial fibrillation. This patient ultimately progressed to complete heart block.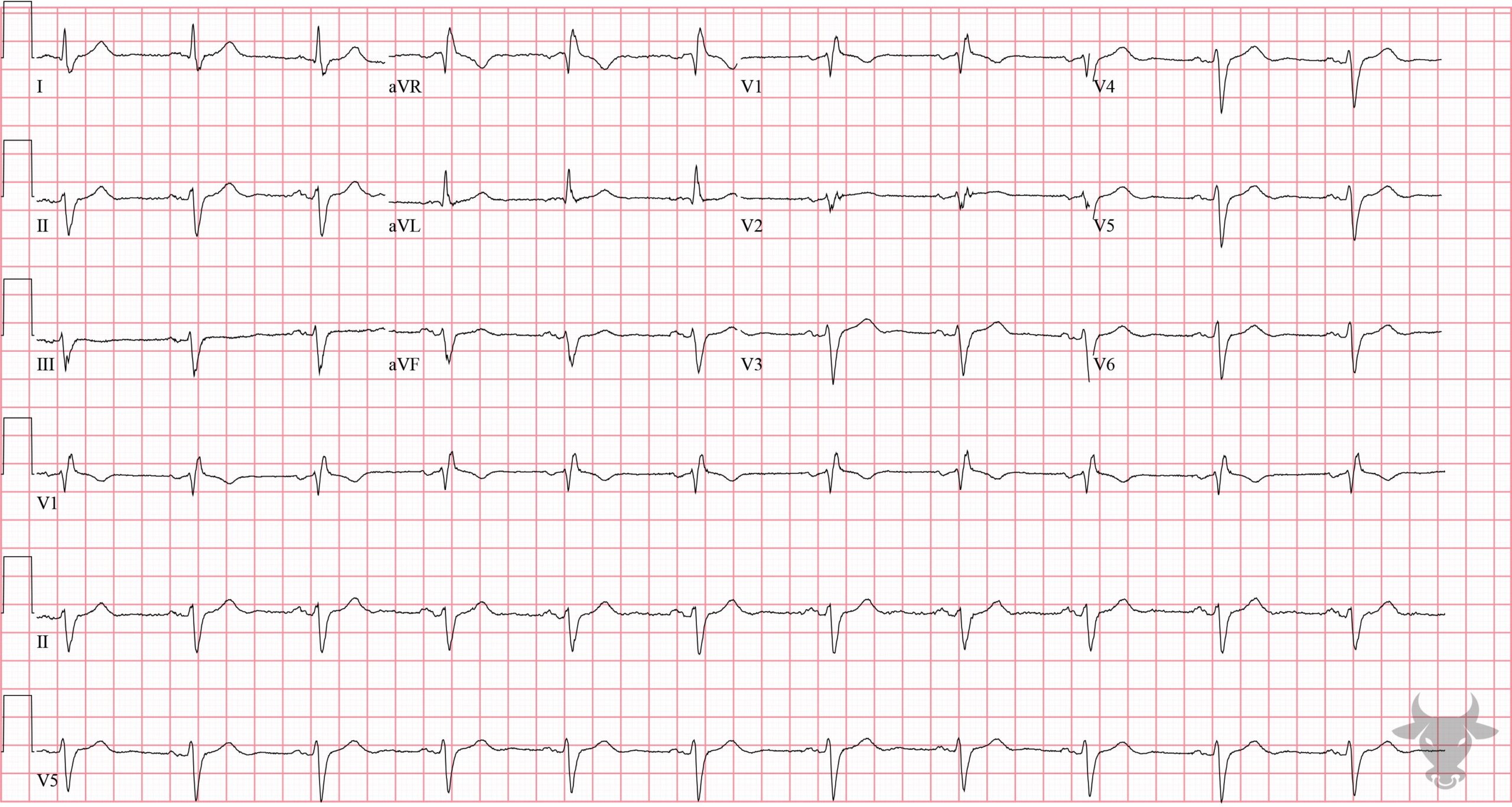
Right Bundle Branch Block & Left Anterior Fascicular Block
Right bundle branch block and left anterior fascicular block.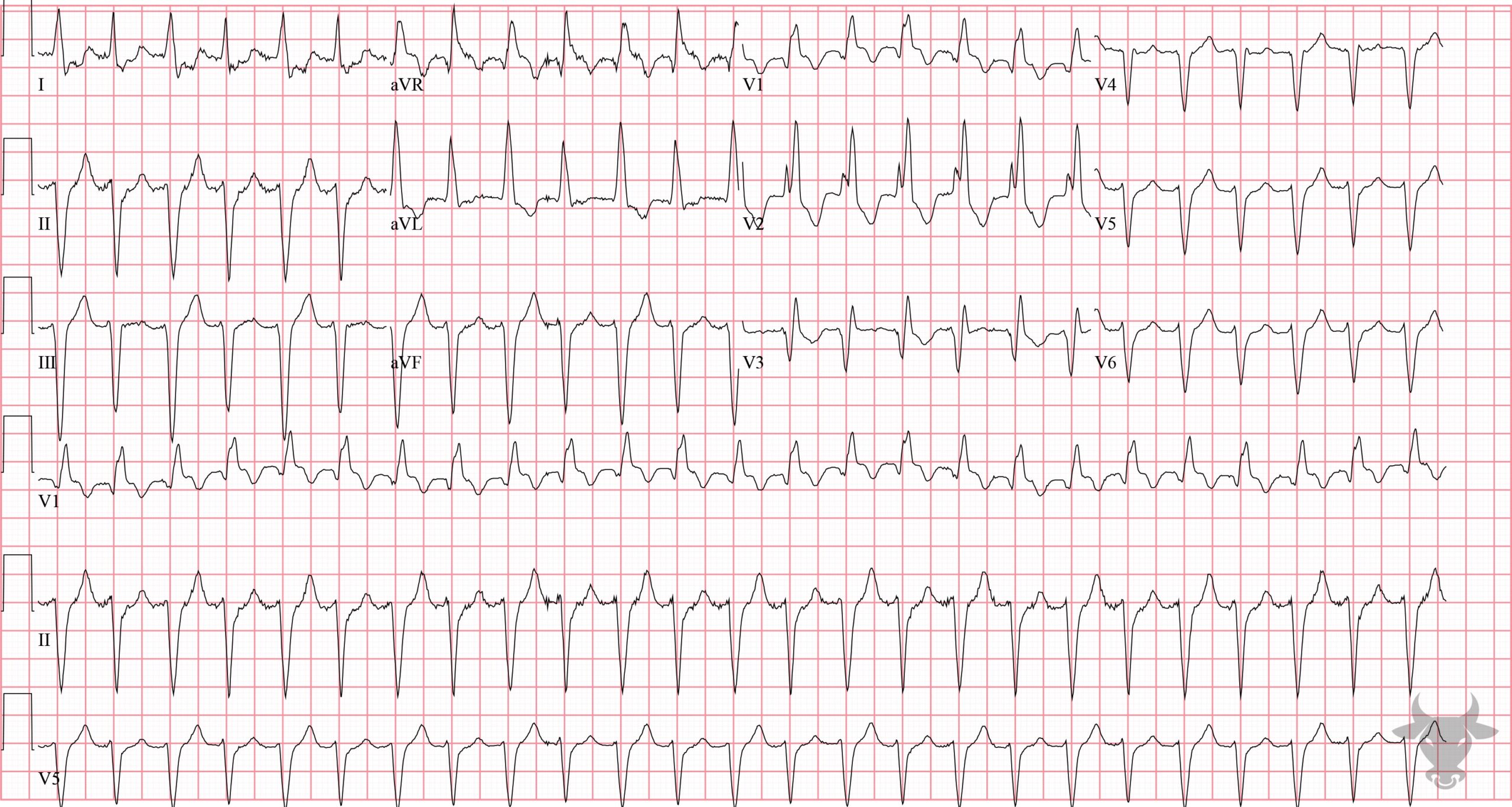
Supraventricular Tachycardia with Aberrancy
Supraventricular tachycardia with aberrancy in a patient with known right bundle branch and left anterior fascicular blocks.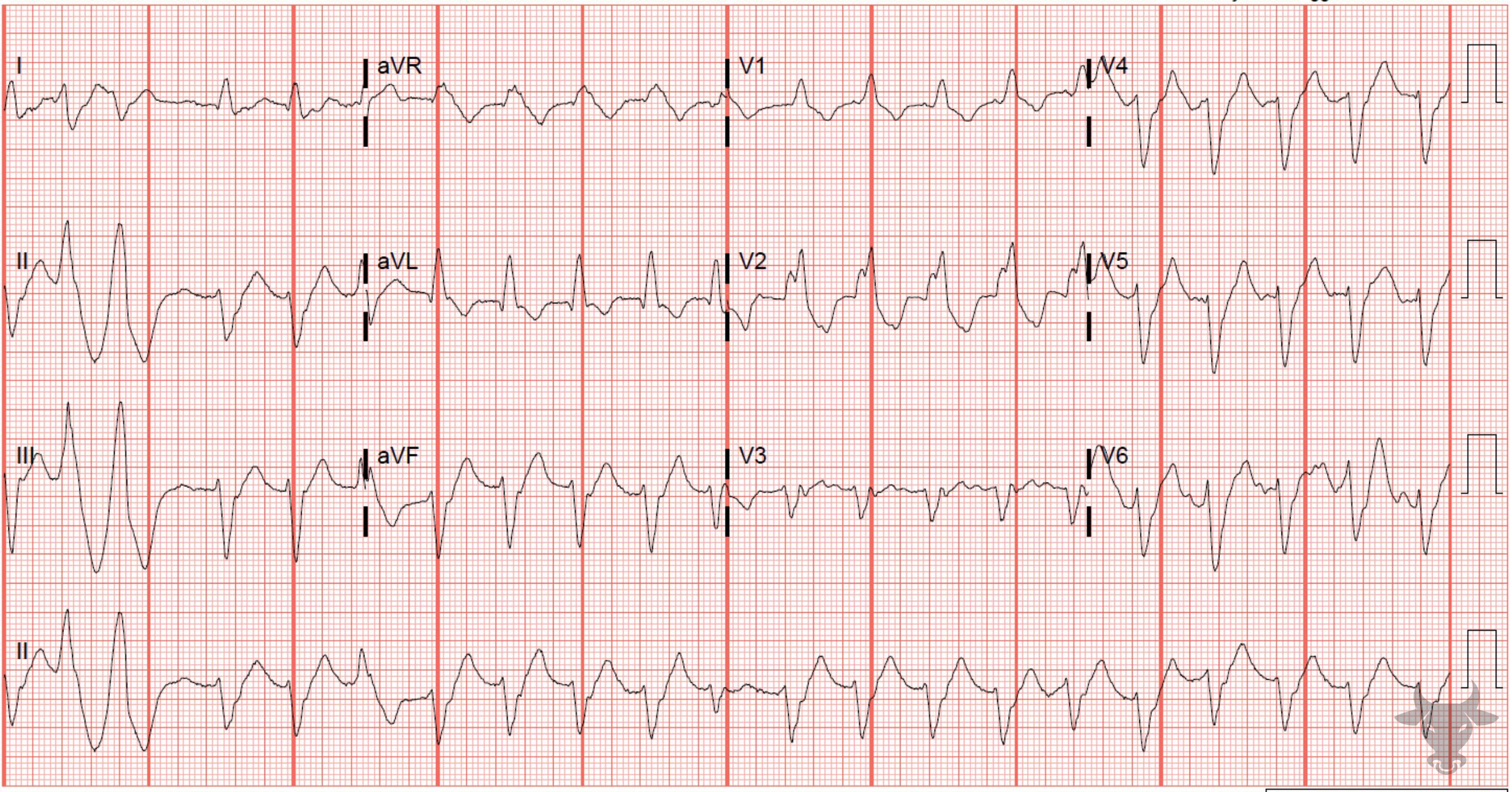
Trifascicular Block
This patient had known trifascicular disease with a right bundle branch block, left anterior fascicular block, and PR prolongation. During tachycardia, even when sinus, trifascicular disease can mimic ventricular tachycardia. At a slower rate, sinus conduction was confirmed.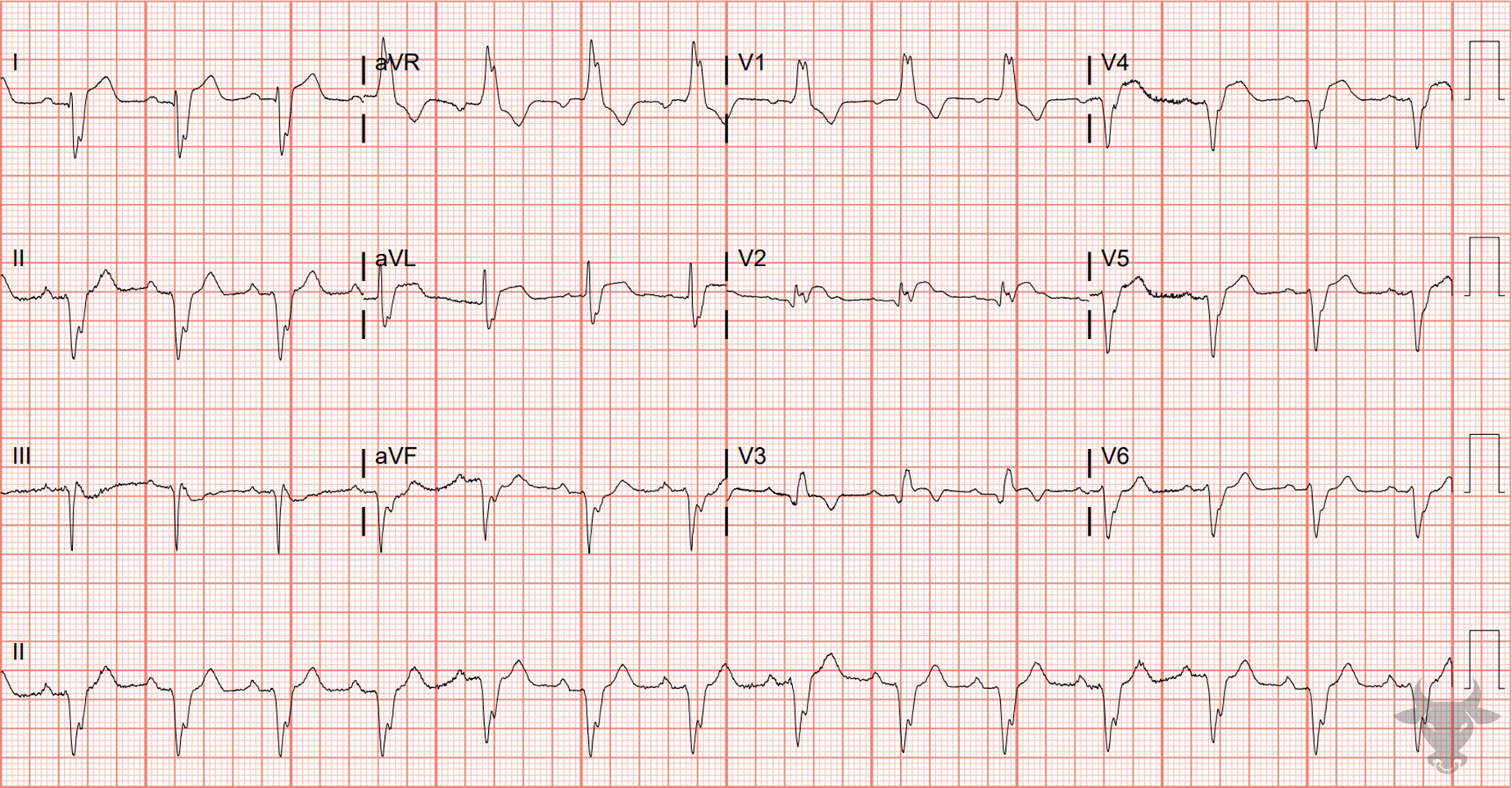
ST-elevation Myocardial Infarction With Right Bundle Branch Block
Typically, a right bundle branch block has either isoelectric or slight ST-segment depressions in the anterior precordial leads (V1 through V3). Any degree of ST-segment elevation in V1 through V3 in the setting of a right bundle branch block is worrisome for acute occlusion. This patient had a left anterior descending artery occlusion.References
- Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhyth. Circulation. 2019;140(8):e382-e482.
- McAnulty JH, Rahimtoola SH, Murphy E, et al. Natural history of “high-risk” bundle-branch block: final report of a prospective study. The New England journal of medicine. 1982;307(3):137-143.
